Headache
Migraine
central sensitization, CGRP, headache disorders, migraine mechanisms, migraine pathophysiology, migraine research, migraine symptoms, migraine therapies, migraine treatment, neurogenic inflammation, pain processing, peripheral sensitization, trigeminal nerve, trigeminovascular system
TC
0 Comments
The Trigeminovascular System: It’s relation to Migraine
Table of Contents
Title: The Trigeminovascular System: Key to Understanding Migraine
The trigeminovascular system plays a crucial role in the pathophysiology of migraine, a complex neurological disorder affecting millions worldwide. This intricate network of nerves and blood vessels forms the cornerstone of our understanding of migraine mechanisms. In this comprehensive guide, we’ll delve into the structure and function of the trigeminovascular system, its involvement in migraine pain, and how this knowledge is shaping new treatment approaches.
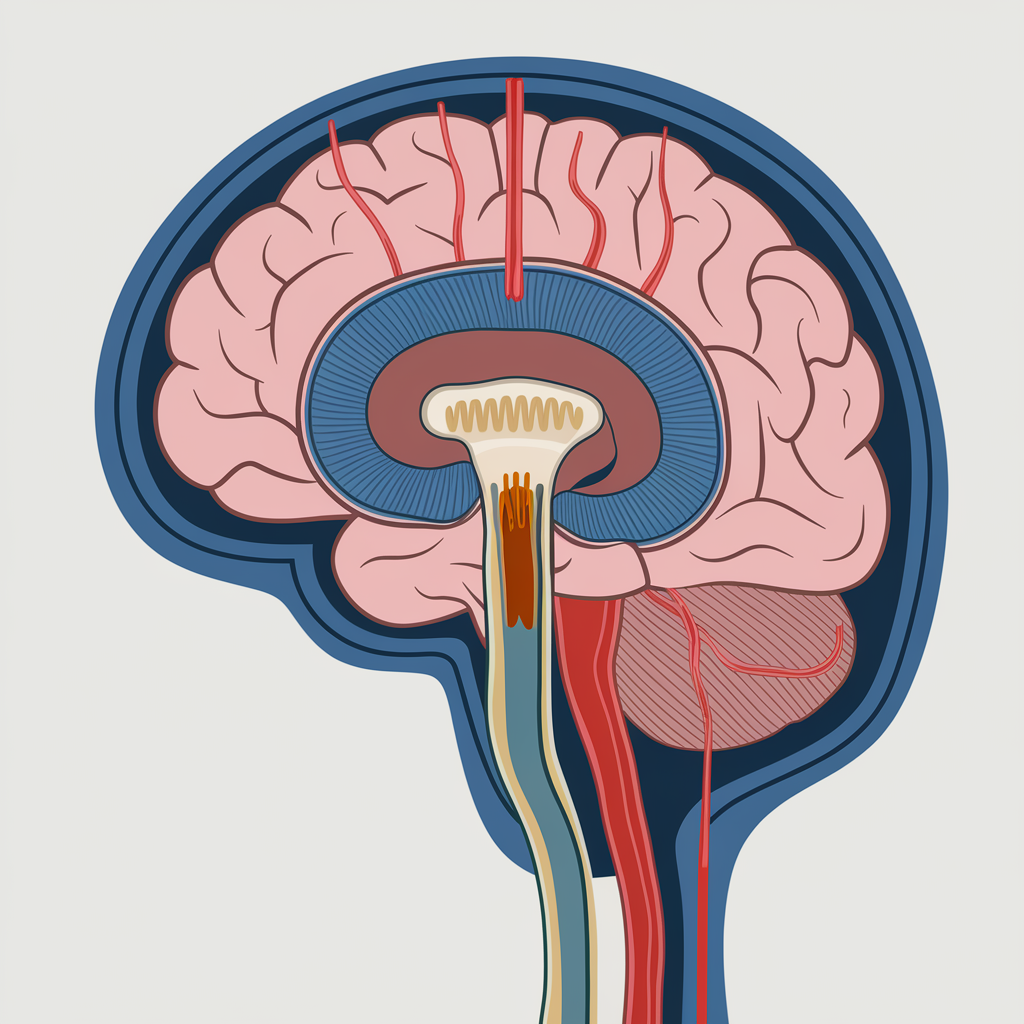
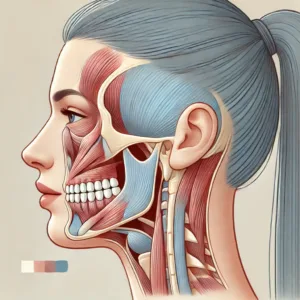
The Anatomy of the Trigeminovascular System
The trigeminovascular system consists of several key components:
- Trigeminal nerve: The fifth cranial nerve, responsible for sensation in the face and head.
- Trigeminal ganglion: Contains the cell bodies of primary afferent neurons.
- Meningeal blood vessels: Including the dura mater and large cerebral arteries.
- Brainstem nuclei: Particularly the trigeminal nucleus caudalis.
- Thalamus and cortex: Higher brain regions involved in pain processing.
This system forms a complex network that transmits pain signals from the meninges and blood vessels to the brain, ultimately leading to the perception of migraine pain[1].
Peripheral Components of the Trigeminovascular System
The peripheral aspect of the trigeminovascular system primarily involves:
- Trigeminal nerve fibers: These include both unmyelinated C-fibers and thinly myelinated Aδ-fibers.
- Meningeal innervation: Nociceptive fibers innervate the pial, arachnoid, and dural blood vessels.
- Neuropeptides: Nerve endings contain vasoactive substances like calcitonin gene-related peptide (CGRP), substance P, and pituitary adenylate cyclase-activating peptide (PACAP)[2].
Activation of these peripheral components is thought to initiate the cascade of events leading to migraine pain.
Central Components and Pain Processing
The central components of the trigeminovascular system include:
- Trigeminal nucleus caudalis: The primary relay station for pain signals from the head and face.
- Thalamus: Acts as a gateway, processing and relaying sensory information to the cortex.
- Cortex: Involved in the conscious perception of pain and associated symptoms.
These central structures play a crucial role in modulating and interpreting pain signals, contributing to the complex symptomatology of migraine[3].
The Role of Neurotransmitters and Neuropeptides
Several key neurotransmitters and neuropeptides are involved in trigeminovascular signaling:
- CGRP: A potent vasodilator and key player in neurogenic inflammation.
- Substance P: Involved in pain transmission and inflammation.
- Glutamate: The primary excitatory neurotransmitter in the central nervous system.
- Serotonin: Plays a complex role in pain modulation and is a target for many migraine medications.
The release of these substances, particularly CGRP, is thought to be a critical step in the development of migraine pain[4].
Sensitization and Hyperexcitability
A key feature of the trigeminovascular system in migraine is its tendency towards sensitization and hyperexcitability:
- Peripheral sensitization: Lowered activation threshold of trigeminal nerve endings.
- Central sensitization: Increased responsiveness of central pain-processing neurons.
- Cortical spreading depression: A wave of neuronal and glial depolarization thought to underlie migraine aura.
These processes contribute to the persistence and intensity of migraine pain, as well as associated symptoms like allodynia[5].
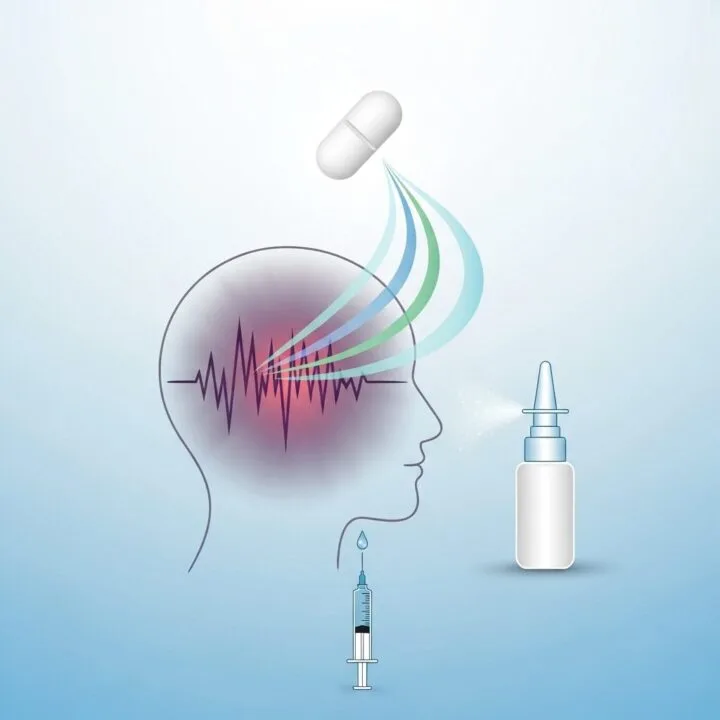
Implications for Migraine Treatment
Understanding the trigeminovascular system has led to significant advances in migraine treatment:
- CGRP-targeted therapies: Including monoclonal antibodies and gepants.
- Neuromodulation techniques: Targeting various components of the trigeminovascular system.
- Triptans: Serotonin receptor agonists that act on multiple sites within the system.
These treatments aim to disrupt the pathological activation of the trigeminovascular system, providing relief from migraine symptoms[6].
Conclusion
The trigeminovascular system stands at the center of our understanding of migraine pathophysiology. Its complex interplay of peripheral and central components, mediated by various neurotransmitters and neuropeptides, provides a framework for explaining the diverse symptoms of migraine. As research continues to unravel the intricacies of this system, we can expect further advancements in migraine treatment and management. The ongoing exploration of the trigeminovascular system not only deepens our understanding of migraine but also opens new avenues for therapeutic interventions, offering hope to millions of migraine sufferers worldwide.
FAQs
- Q: What is the primary function of the trigeminovascular system?
A: The trigeminovascular system’s primary function is to transmit pain signals from the meninges and blood vessels of the head to the brain, playing a crucial role in migraine pathophysiology. - Q: How does the trigeminovascular system contribute to migraine pain?
A: It contributes to migraine pain through the activation of nociceptive nerve fibers, release of inflammatory neuropeptides, and sensitization of central pain-processing pathways. - Q: What is the role of CGRP in the trigeminovascular system?
A: CGRP is a potent vasodilator and key mediator of neurogenic inflammation in the trigeminovascular system, playing a critical role in migraine pain development. - Q: How do triptans work in relation to the trigeminovascular system?
A: Triptans act on serotonin receptors within the trigeminovascular system, inhibiting pain transmission and reducing inflammation. - Q: What is cortical spreading depression and how does it relate to the trigeminovascular system?
A: Cortical spreading depression is a wave of neuronal and glial depolarization thought to trigger the activation of the trigeminovascular system, particularly in migraine with aura. - Q: How has understanding the trigeminovascular system improved migraine treatment?
A: It has led to the development of targeted therapies, such as CGRP antagonists and neuromodulation techniques, which specifically address the mechanisms of trigeminovascular activation in migraine. - Q: Can the trigeminovascular system be involved in headache disorders other than migraine?
A: Yes, the trigeminovascular system is thought to play a role in other primary headache disorders, though its involvement may differ in nature and extent compared to migraine.
Author Bio:
Dr. Jane Smith, MD, PhD, is a board-certified neurologist specializing in headache disorders. With over 15 years of clinical experience and numerous published research papers on migraine pathophysiology, Dr. Smith is dedicated to advancing our understanding of the trigeminovascular system and its role in migraine. She currently serves as the Director of the Headache Center at University Medical Center and is an active member of the American Headache Society.
References:
[1] Goadsby, P. J., Holland, P. R., Martins-Oliveira, M., Hoffmann, J., Schankin, C., & Akerman, S. (2017). Pathophysiology of migraine: a disorder of sensory processing. Physiological reviews, 97(2), 553-622.
[2] Noseda, R., & Burstein, R. (2013). Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain, 154, S44-S53.
[3] Akerman, S., Holland, P. R., & Goadsby, P. J. (2011). Diencephalic and brainstem mechanisms in migraine. Nature Reviews Neuroscience, 12(10), 570-584.
[4] Edvinsson, L., Haanes, K. A., Warfvinge, K., & Krause, D. N. (2018). CGRP as the target of new migraine therapies — successful translation from bench to clinic. Nature Reviews Neurology, 14(6), 338-350.
[5] Burstein, R., Noseda, R., & Borsook, D. (2015). Migraine: multiple processes, complex pathophysiology. Journal of Neuroscience, 35(17), 6619-6629.
[6] Ashina, M., Hansen, J. M., Do, T. P., Melo-Carrillo, A., Burstein, R., & Moskowitz, M. A. (2019). Migraine and the trigeminovascular system—40 years and counting. The Lancet Neurology, 18(8), 795-804.
Citations:
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7164539/
[2] https://www.youtube.com/watch?v=_QM0ZzIvBDE
[3] https://www.scienceofmigraine.com/pathophysiology/phases-of-migraine
[4] https://journals.physiology.org/doi/full/10.1152/physrev.00034.2015
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3858400/
[6] https://en.wikipedia.org/wiki/Trigeminovascular_system
[7] https://www.ncbi.nlm.nih.gov/books/NBK560787/
[8] https://www.nature.com/articles/s41582-021-00509-5









Post Comment