Temporomandibular Joint Surgery: Procedures, Indications, and Outcomes
Table of Contents
Temporomandibular Joint Surgery: Procedures, Indications, and Outcomes
Introduction
Temporomandibular joint (TMJ) disorders affect a significant portion of the population, with estimates ranging from 5% to 12%. While conservative management remains the first-line approach, surgical intervention may be necessary for refractory cases. This article provides a comprehensive overview of TMJ surgical procedures, their indications, and evidence-based outcomes.
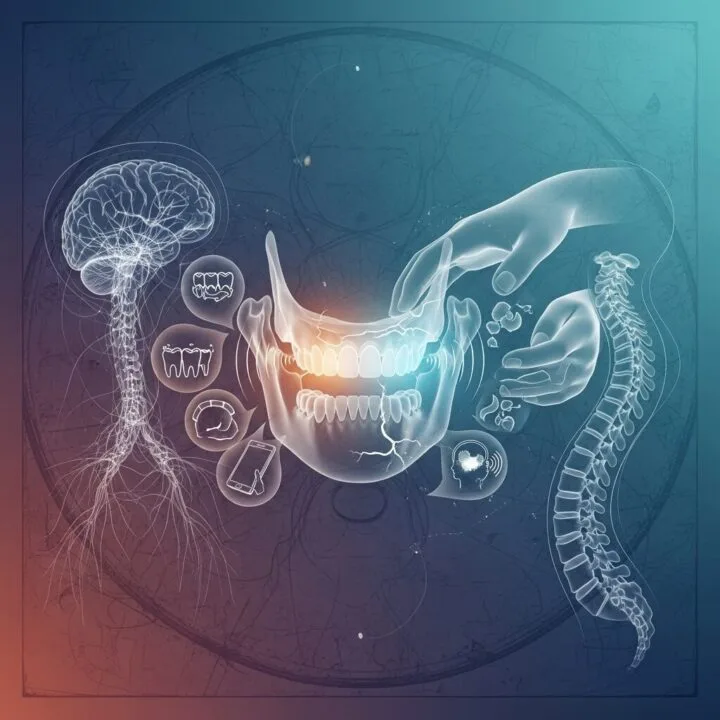
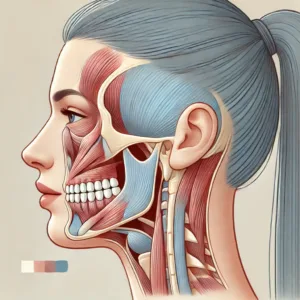
Anatomy and Pathophysiology of the Temporomandibular Joint
The temporomandibular joint is a complex synovial joint that allows for both rotational and translational movements. It consists of the mandibular condyle, articular disc, and glenoid fossa of the temporal bone. TMJ disorders can arise from various etiologies, including:
- Osteoarthritis
- Internal derangement
- Synovitis
- Adhesions
- Ankylosis
Understanding the underlying pathology is crucial for selecting appropriate surgical interventions.
Diagnostic Imaging in TMJ Disorders
Accurate diagnosis is essential for surgical planning. Common imaging modalities include:
- Panoramic radiography
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Cone-beam computed tomography (CBCT)
MRI is particularly useful for evaluating soft tissue structures, while CT provides detailed information about bony anatomy.
Minimally Invasive Procedures
Arthrocentesis
Arthrocentesis is a minimally invasive procedure that involves lavage of the joint space.
Indications:
- Acute closed lock
- Disc displacement without reduction
- Osteoarthritis with effusion
Procedure:
- Two needles are inserted into the superior joint space
- Sterile solution is used to lavage the joint
- Hydraulic pressure is applied to release adhesions
Outcomes:
A systematic review by Al-Moraissi (2015) found that arthrocentesis significantly improved maximum mouth opening and pain scores in patients with TMJ disorders.
Arthroscopy
TMJ arthroscopy allows for direct visualization and treatment of intra-articular pathology.
Indications:
- Internal derangement
- Synovitis
- Adhesions
Procedure:
- A small incision is made for the arthroscope
- Additional portals may be created for instrumentation
- Procedures such as lysis of adhesions or disc repositioning can be performed
Outcomes:
Gonzalez-Garcia et al. (2018) reported significant improvements in pain and function following arthroscopic procedures, with success rates ranging from 80% to 90%.
Open Joint Procedures
Arthroplasty
Arthroplasty involves surgical modification of the joint surfaces.
Indications:
- Advanced osteoarthritis
- Ankylosis
- Failed minimally invasive procedures
Types of Arthroplasty:
- Condylectomy
- Eminectomy
- Discectomy with or without replacement
Outcomes:
A long-term follow-up study by Dimitroulis (2011) showed that discectomy without replacement provided satisfactory outcomes in 85% of patients at 15 years post-surgery.
Total Joint Replacement
Total joint replacement is reserved for end-stage TMJ disease.
Indications:
- Severe degenerative joint disease
- Congenital malformations
- Failed previous surgeries
Procedure:
- Removal of diseased joint components
- Placement of prosthetic fossa and condyle
Outcomes:
Wolford et al. (2016) reported significant improvements in pain, function, and quality of life following total joint replacement, with a 95% implant survival rate at 10 years.
Perioperative Considerations
Patient Selection
Careful patient selection is crucial for surgical success. Factors to consider include:
- Age and overall health
- Previous treatments and their outcomes
- Psychosocial factors
- Realistic expectations
Anesthesia
TMJ surgery can be performed under general anesthesia or local anesthesia with sedation. The choice depends on the procedure complexity and patient factors.
Post-operative Management
Post-operative care is critical for optimal outcomes:
- Pain management
- Physical therapy
- Dietary modifications
- Occlusal splint therapy
Complications and Their Management
Potential complications of TMJ surgery include:
- Infection
- Nerve injury
- Malocclusion
- Ankylosis
- Implant failure (in total joint replacement)
Early recognition and appropriate management of complications are essential for minimizing long-term sequelae.
Emerging Technologies and Future Directions
Recent advancements in TMJ surgery include:
- 3D-printed patient-specific implants
- Tissue engineering approaches for disc regeneration
- Robotic-assisted surgery
These technologies show promise in improving surgical precision and patient outcomes.
Conclusion
Temporomandibular joint surgery encompasses a range of procedures, from minimally invasive techniques to complex reconstructions. While surgical intervention can provide significant relief for refractory TMJ disorders, it should be considered only after conservative measures have failed. Careful patient selection, appropriate surgical technique, and comprehensive post-operative care are crucial for achieving optimal outcomes.
FAQs
- What is the success rate of TMJ arthroscopy?
Studies report success rates between 80-90% for arthroscopic procedures in appropriately selected patients. - How long is the recovery period after open TMJ surgery?
Recovery can take 6-8 weeks for basic function, with full recovery potentially taking several months. - Are there age restrictions for TMJ surgery?
While there are no strict age limits, the risks and benefits must be carefully weighed, especially in growing patients or older adults with comorbidities. - Can TMJ surgery improve limited mouth opening?
Yes, many patients experience improved mouth opening following surgery, particularly in cases of disc displacement or adhesions. - What is the longevity of total TMJ prostheses?
Current literature suggests a 10-year survival rate of approximately 90-95% for modern TMJ prostheses.










Post Comment