Temporomandibular Joint Disorder (TMD) Risk Factors: A Comprehensive Review
Table of Contents
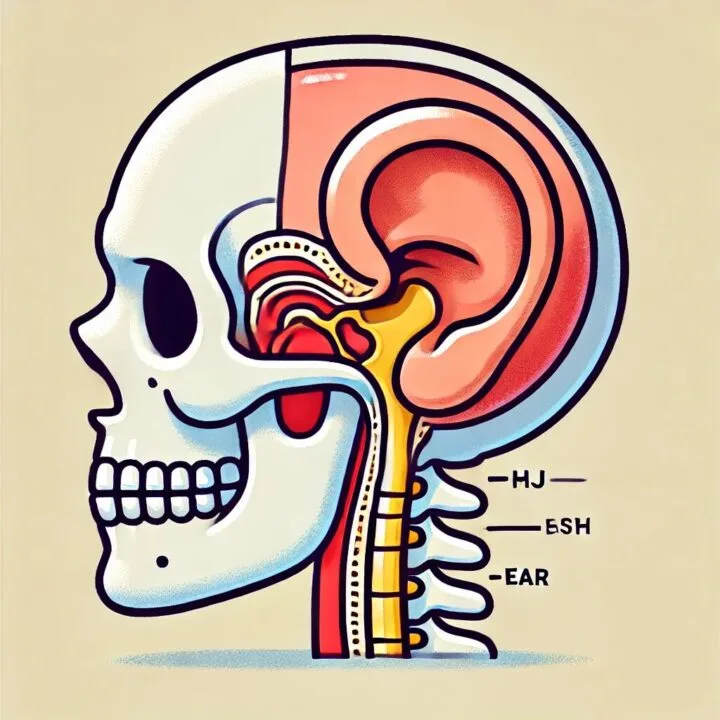
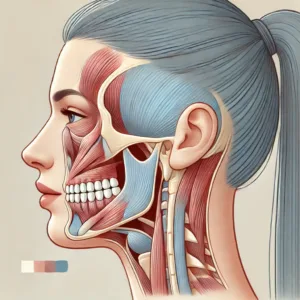
Temporomandibular joint disorders (TMDs) are a group of conditions affecting the temporomandibular joint (TMJ) and associated structures. These disorders are characterized by pain, limited jaw movement, and joint sounds, significantly impacting patients’ quality of life. The etiology of TMDs is multifactorial, involving a complex interplay of biological, psychological, and social factors. This review aims to provide an updated overview of the risk factors associated with TMDs, based on current scientific evidence.
Epidemiological Factors
TMDs are prevalent conditions, with studies estimating that approximately 36% of adults aged 20-49 years experience painful TMD (myalgia and/or arthralgia)[1]. The condition predominantly affects women, with a female-to-male ratio of approximately 2:1[2]. The peak incidence occurs between 20 and 40 years of age, with a gradual decline thereafter[3].
Genetic Predisposition
Recent research has identified genetic factors that may contribute to TMD susceptibility. Studies have suggested variations in genes related to pain processing and inflammation may play a role in TMD development[4]. For instance, estrogen receptor polymorphisms have been associated with an increased risk of TMD, potentially explaining the higher prevalence in women[5].
Hormonal Influences
The higher prevalence of TMDs in women has led researchers to investigate the role of hormonal factors. Estrogen, in particular, has been implicated in TMD pathogenesis. Fluctuations in estrogen levels during the menstrual cycle, pregnancy, and menopause have been associated with changes in TMD symptoms[6]. Additionally, the use of oral contraceptives has been linked to an increased risk of TMD development in some studies[7].
Psychosocial Factors
Psychological and social factors play a significant role in TMD risk and symptom severity. Stress, anxiety, and depression have been consistently linked to increased TMD risk and symptom exacerbation[8]. The OPPERA (Orofacial Pain: Prospective Evaluation and Risk Assessment) study, a large-scale prospective cohort study, found that psychological factors, including somatic awareness, psychosocial stress, and negative affect, were associated with an increased risk of developing TMD.
Biomechanical Factors
Several biomechanical factors have been implicated in TMD development:
- Occlusal discrepancies: While the role of occlusion in TMD etiology remains controversial, some studies suggest that certain occlusal factors, such as posterior crossbite and large overjet, may contribute to TMD risk.
- Bruxism: Both awake and sleep bruxism have been associated with an increased risk of TMD. The repetitive loading of the TMJ and masticatory muscles during bruxism may lead to tissue damage and pain.
- Joint hypermobility: Generalized joint hypermobility has been linked to an increased risk of TMD, possibly due to altered joint biomechanics and increased susceptibility to tissue damage.
Trauma
Macrotrauma, such as direct impact to the jaw or whiplash injuries, has been associated with an increased risk of TMD development. A study by Lee et al. found that facial trauma was a significant risk factor for TMD, with patients experiencing maxillofacial injuries showing a high incidence of TMD symptoms even without condylar fractures.
Central Sensitization
Alterations in central pain processing mechanisms have been implicated in chronic TMD. Central sensitization, characterized by increased responsiveness of nociceptive neurons in the central nervous system, may contribute to the persistence and spread of pain in TMD patients. This phenomenon may explain why some individuals develop chronic TMD while others experience only acute symptoms.
Comorbid Conditions
Several comorbid conditions have been associated with an increased risk of TMD:
- Fibromyalgia: Patients with fibromyalgia have a higher prevalence of TMD compared to the general population, suggesting shared pathophysiological mechanisms.
- Headaches: Migraine and tension-type headaches are more common in TMD patients, and their presence may increase the risk of TMD development.
- Other pain conditions: Widespread pain conditions, such as low back pain and irritable bowel syndrome, have been associated with an increased risk of TMD.
Environmental and Lifestyle Factors
Various environmental and lifestyle factors may contribute to TMD risk:
- Occupation: Certain occupations that involve prolonged jaw positioning or exposure to vibration may increase TMD risk.
- Diet: While evidence is limited, some studies suggest that a diet high in processed foods and low in omega-3 fatty acids may contribute to TMD risk.
- Sleep disturbances: Poor sleep quality and sleep disorders have been associated with an increased risk of TMD and may exacerbate existing symptoms.
Conclusion
The etiology of TMDs is complex and multifactorial, involving a wide range of biological, psychological, and social factors. Understanding these risk factors is crucial for developing effective prevention strategies and targeted interventions. Future research should focus on elucidating the specific causal pathways and interactions between these factors to improve our understanding of TMD pathogenesis and guide the development of personalized treatment approaches.
As our knowledge of TMD risk factors continues to evolve, it is essential to adopt a comprehensive, biopsychosocial approach to TMD assessment and management. Clinicians should consider the full spectrum of potential risk factors when evaluating and treating patients with TMD, recognizing that individual patients may have unique combinations of contributing factors.
References:
- Slade GD, et al. J Pain. 2011;12(11 Suppl):T37-T45.
- LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8(3):291-305.
- Manfredini D, et al. J Oral Rehabil. 2010;37(3):150-162.
- Smith SB, et al. Pain. 2011;152(10):2295-2303.
- Ribeiro-Dasilva MC, et al. J Pain. 2009;10(9):944-952.
- Warren MP, Fried JL. J Am Dent Assoc. 2001;132(1):49-57.
- Maixner W, et al. J Pain. 2011;12(11 Suppl):T102-T115.
- Fillingim RB, et al. J Pain. 2011;12(11 Suppl):T46-T56.
- Slade GD, et al. J Pain. 2016;17(12):1261-1270.
- Pullinger AG, Seligman DA. J Orofac Pain. 2000;14(3):187-201.
- Manfredini D, Lobbezoo F. J Oral Rehabil. 2010;37(1):1-23.
- Kavuncu V, et al. Rheumatol Int. 2006;26(3):257-260.
- Häggman-Henrikson B, et al. J Oral Rehabil. 2014;41(7):469-480.
- Lee YH, et al. Med Sci Monit. 2018;24:4739-4746.
- Woolf CJ. Pain. 2011;152(3 Suppl):S2-15.
- Plesh O, et al. J Rheumatol. 1996;23(11):1948-1952.
- Speciali JG, Dach F. Headache. 2015;55 Suppl 1:72-83.
- Velly AM, et al. J Pain. 2010;11(12):1311-1319.
- Nishiyama A, et al. J Oral Rehabil. 2012;39(5):323-333.
- Lobo SL, et al. J Orofac Pain. 2014;28(1):61-70.
- Sanders AE, et al. Sleep. 2013;36(7):1017-1025.
Citations:
[1] https://www.medecinesciences.org/en/articles/medsci/full_html/2018/09/medsci180268s/medsci180268s.html
[2] https://www.sciencedirect.com/science/article/abs/pii/S2212440323000329
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8492627/
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4689239/
[5] https://www.doctortmj.com/tmj-blog/what-groups-are-at-risk-for-tmj/
[6] https://www.ncbi.nlm.nih.gov/books/NBK551612/
[7] https://www.isleepsolutions.com/risk-factors-of-tmj.html
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10643880/









Post Comment