Temporomandibular Joint Disorder (TMD): A Comprehensive Review of Epidemiology, Etiology, Diagnosis, and Management
Temporomandibular Joint Disorder (TMD): A Comprehensive Review of Epidemiology, Etiology, Diagnosis, and Management
Abstract
Temporomandibular joint disorder (TMD) is a complex musculoskeletal condition characterized by pain, limited jaw movement, and joint sounds, significantly impacting patients’ quality of life. This review aims to provide an updated overview of TMD’s epidemiology, etiology, diagnosis, and management, highlighting the current understanding and future directions in TMD research.
Epidemiology
TMD is a prevalent condition, affecting approximately 36% of adults aged 20-49 years, with a female-to-male ratio of approximately 2:1. The peak incidence occurs between 20 and 40 years of age, with a gradual decline thereafter.
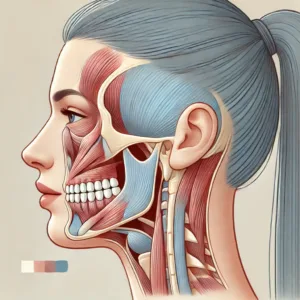
Etiology and Pathophysiology
The etiology of TMD is multifactorial, involving a complex interplay of biological, psychological, and social factors. Recent research has identified several potential contributing factors, including:
- Genetic predisposition: Variations in genes related to pain processing and inflammation have been associated with TMD susceptibility.
- Hormonal influences: Estrogen receptor polymorphisms have been linked to an increased risk of TMD, potentially explaining the higher prevalence in women.
- Psychosocial factors: Stress, anxiety, and depression have been associated with increased TMD risk and symptom severity.
- Biomechanical factors: Occlusal discrepancies, bruxism, and joint hypermobility may contribute to TMD development.
- Central sensitization: Alterations in central pain processing mechanisms have been implicated in chronic TMD.
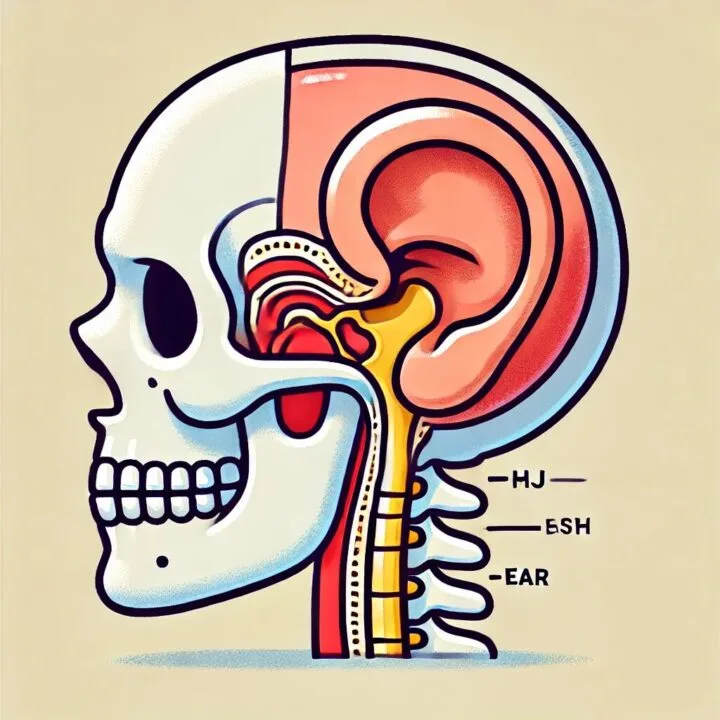
The pathophysiology of TMD involves both peripheral and central mechanisms. Peripheral sensitization of nociceptors in the TMJ and masticatory muscles can lead to localized pain and dysfunction, while central sensitization may result in widespread pain and hyperalgesia.
Diagnosis
Accurate diagnosis of TMD is crucial for effective management. The Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) is the current gold standard for TMD diagnosis in both clinical and research settings. The DC/TMD includes:
- Axis I: Physical assessment: Evaluation of myalgia, arthralgia, headache attributed to TMD, disc displacements, degenerative joint disease, and subluxation.
- Axis II: Psychosocial assessment: Assessment of pain-related disability, psychological distress, and pain catastrophizing.
Clinical examination should include palpation of masticatory muscles and TMJ, assessment of mandibular range of motion, and evaluation of joint sounds. Imaging modalities such as panoramic radiography, computed tomography (CT), and magnetic resonance imaging (MRI) may be used to assess joint morphology and disc position, but their routine use is not recommended for initial diagnosis.
Management
Management of TMD should follow a conservative, multidisciplinary approach, tailored to the individual patient’s needs. Current evidence supports the following interventions:
- Patient education and self-management: Educating patients on the benign nature of most TMDs and providing strategies for symptom management.
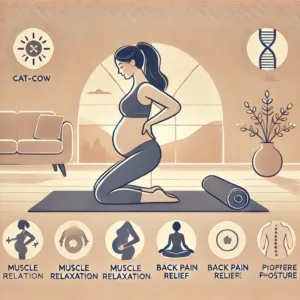
- Physical therapy: Exercises to improve jaw mobility, posture correction, and manual therapy techniques.
- Occlusal appliances: Using occlusal splints to reduce TMD symptoms, particularly in patients with bruxism.
- Pharmacotherapy: Nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants may provide short-term pain relief, while tricyclic antidepressants have shown efficacy in managing chronic TMD pain.
- Cognitive-behavioral therapy (CBT): CBT has demonstrated effectiveness in managing chronic TMD pain and associated psychological distress.
- Minimally invasive procedures: Arthrocentesis and arthroscopy may be considered for patients with persistent symptoms refractory to conservative management.
- Surgical interventions: Reserved for severe cases with significant structural abnormalities or those unresponsive to conservative measures.
Future Directions
Emerging research in TMD focuses on:
- Personalized medicine approaches: Tailoring treatment to an individual’s genetic and molecular profile.
- Novel pharmacological targets: Investigating cannabinoid receptors and ion channels involved in pain signaling.
- Advanced imaging techniques: Developing early detection methods for TMJ degeneration.
- Tissue-engineered TMJ replacements: Creating innovative, effective treatments for TMD.
In conclusion, TMD is a complex condition requiring a comprehensive understanding of its multifactorial etiology and the application of evidence-based, patient-centered approaches for optimal outcomes. Future research should focus on elucidating specific causal pathways and developing targeted, mechanism-based interventions.









Post Comment