What Causes Perimenopause Shoulder Pain and How Can You Relieve It?
Table of Contents

What Causes Perimenopause Shoulder Pain and How Can You Relieve It?
Introduction
Are you in your 40s or 50s and suddenly experiencing unexplained shoulder pain? If you’re navigating through perimenopause, this discomfort could be one of its lesser-known symptoms. Perimenopause shoulder pain is more common than many realize and can significantly impact daily life, making tasks like lifting objects or even sleeping difficult.
In this article, we’ll explore why perimenopause can cause shoulder pain, how to distinguish it from other issues, and most importantly, what you can do to manage and relieve it effectively.
What Is Perimenopause, and How Can It Affect Joints and Muscles?
1. What Happens During Perimenopause?
Perimenopause marks the transition period before menopause, typically occurring between the ages of 40 and 55. Hormonal fluctuations, particularly a decline in estrogen, play a significant role in triggering a wide range of symptoms.
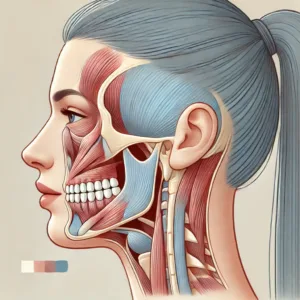
2. Why Does Perimenopause Affect Shoulder Joints?
Estrogen has a protective role in maintaining healthy joints and muscles by reducing inflammation and promoting collagen production. When estrogen levels drop during perimenopause, the following effects can lead to shoulder pain:
- Increased inflammation: The body may experience more widespread inflammation, affecting the joints and surrounding tissues.
- Weakened tendons and ligaments: With less collagen production, tendons and ligaments become less elastic and more prone to strain.
- Muscle stiffness: Hormonal imbalances can cause overall muscle tension, leading to shoulder pain and stiffness.
What Are the Common Causes of Shoulder Pain During Perimenopause?
1. Hormonal Imbalance and Inflammation
The fluctuating levels of estrogen, progesterone, and other hormones can create an inflammatory environment in the body. This inflammation often manifests as:
- Frozen shoulder (adhesive capsulitis): Characterized by stiffness and reduced range of motion.
- Tendonitis: Inflammation of the tendons around the shoulder, causing pain with movement.
- Bursitis: Inflammation of the small sacs of fluid (bursae) that cushion the joints.
2. Muscle Tension from Stress
Perimenopause often brings emotional challenges such as mood swings, anxiety, and stress. These can lead to muscle tension and tightness, particularly in the neck and shoulders.
3. Osteoarthritis and Joint Degeneration
The natural wear and tear of joints, combined with reduced estrogen levels, can accelerate the progression of osteoarthritis in the shoulder joint, causing chronic pain and limited mobility.
How Can You Relieve Shoulder Pain from Perimenopause?
1. Can Stretching and Strengthening Exercises Help?
Yes! Regular, gentle exercises can reduce stiffness, improve circulation, and promote joint health.
Try these simple exercises:
- Shoulder rolls: Roll your shoulders forward and backward to relieve tension.
- Wall crawls: Stand near a wall and “crawl” your fingers up as high as you can to improve flexibility.
- Resistance band exercises: Strengthen the rotator cuff and surrounding muscles with light resistance exercises.
2. Should You Apply Heat or Cold Compresses?
Both heat and cold therapy can be effective, depending on the nature of your pain.
- Cold compress: Reduces inflammation and numbs sharp pain.
- Heat therapy: Relaxes tight muscles and improves blood flow.
Pro Tip: Alternate between cold and heat for 10-15 minutes each to maximize relief.
3. What Role Do Anti-Inflammatory Foods Play?
Your diet can either contribute to or help combat inflammation. Including anti-inflammatory foods can reduce pain and promote joint health.
Recommended foods:
- Fatty fish (salmon, mackerel)
- Turmeric (curcumin)
- Leafy greens (spinach, kale)
- Berries (blueberries, strawberries)
4. Are There Over-the-Counter Remedies That Help?
Non-prescription options like NSAIDs (ibuprofen or naproxen) can temporarily relieve inflammation and pain.
Important: Long-term use should be discussed with a healthcare professional to avoid side effects.
5. Can Hormone Replacement Therapy (HRT) Provide Long-Term Relief?
Hormone replacement therapy can help restore hormonal balance, potentially reducing inflammation and muscle stiffness.
Consult your doctor to discuss whether HRT is suitable for you based on your medical history.
When Should You See a Doctor?
1. What Are the Signs of Severe or Chronic Shoulder Issues?
If your shoulder pain persists for more than a few weeks or is accompanied by any of the following, seek medical advice:
- Swelling or redness
- Loss of range of motion
- Persistent stiffness or pain that worsens over time
- Numbness or tingling in the arm or hand
2. Could It Be a Sign of an Underlying Condition?
Persistent shoulder pain may indicate conditions like:
- Frozen shoulder: Characterized by severe stiffness and limited movement.
- Rotator cuff injury: May require physical therapy or surgical intervention.
- Rheumatoid arthritis: An autoimmune condition that can affect multiple joints.
Preventive Tips to Manage Shoulder Pain During Perimenopause
1. How Can Posture Play a Role in Shoulder Health?
Maintaining proper posture reduces strain on the shoulder muscles and joints.
Posture tips:
- Avoid slouching when sitting.
- Use ergonomic support at your workstation.
- Take regular breaks to stretch if you sit for long periods.
2. Can Stress Management Techniques Help?
Reducing stress can lower muscle tension and inflammation, indirectly helping shoulder pain.
Effective stress-relieving techniques:
- Yoga or tai chi
- Meditation or deep breathing exercises
- Regular physical activity
3. Why Is Staying Active Important?
Regular physical activity improves joint mobility, muscle strength, and circulation, which can prevent stiffness and reduce pain.
Conclusion
Shoulder pain during perimenopause is a common issue that can significantly affect your quality of life. Fortunately, by understanding the role of hormonal changes and inflammation, you can take proactive steps to manage and prevent this discomfort. Incorporating stretching, anti-inflammatory foods, proper posture, and stress management into your daily routine can make a noticeable difference.
If the pain persists or worsens, don’t hesitate to seek professional medical advice to identify any underlying conditions and develop a comprehensive treatment plan.
FAQ
1. Can shoulder pain be an early symptom of perimenopause?
Yes, hormonal changes during perimenopause can lead to inflammation and muscle stiffness, contributing to shoulder pain.
2. How long does perimenopause shoulder pain last?
The duration can vary. For some, it may last only a few weeks, while others may experience it throughout the perimenopausal phase.
3. Are natural remedies effective for shoulder pain?
Yes, natural remedies like turmeric, omega-3 fatty acids, and yoga can help reduce inflammation and relieve pain.
4. Can sleeping positions worsen shoulder pain?
Yes, sleeping on the affected side or using an improper pillow can increase strain on the shoulder. Consider using an orthopedic pillow.
5. Will exercise make my shoulder pain worse?
Gentle, targeted exercises can relieve pain, but high-impact or strenuous activities may worsen it. Always consult a physical therapist if unsure.











Post Comment