The Complex Pathophysiology of Migraine: A Comprehensive Overview
Table of Contents

Migraine is a complex neurological disorder characterized by recurrent episodes of moderate to severe headache, often accompanied by sensory disturbances and other symptoms. Affecting more than one billion people worldwide, migraine stands as the sixth most common cause of disability globally. The pathophysiology of migraine involves intricate interactions between various brain regions, neurotransmitters, and sensory processing systems. This article delves into the current understanding of migraine pathophysiology, exploring its genetic basis, neuroanatomical pathways, and the mechanisms underlying its various phases.
Genetic Foundations of Migraine
Migraine has a strong genetic component, with multiple genes contributing to susceptibility. Family studies have consistently shown that migraine tends to run in families, with first-degree relatives of migraine sufferers having a significantly higher risk of developing the disorder. Recent genome-wide association studies (GWAS) have identified numerous genetic loci associated with migraine risk, shedding light on the complex genetic architecture of the disorder.Key genetic findings include:
- Mutations in the CACNA1A gene, which encodes a subunit of neuronal calcium channels, are associated with familial hemiplegic migraine type 1 (FHM1).
- Variants in genes related to neurotransmitter systems, including serotonin and glutamate pathways, have been implicated in migraine susceptibility.
- Genetic factors influencing vascular function and pain processing pathways have also been identified as contributors to migraine risk.
Understanding the genetic basis of migraine not only helps explain its hereditary nature but also provides potential targets for novel therapeutic interventions.
The Migraine Brain: Altered Sensory Processing
Migraine is now understood to be a disorder of brain function rather than simply a vascular condition. The migraine brain exhibits altered sensory processing and regulation of signals, particularly those originating in the head. This dysregulation involves several key areas:
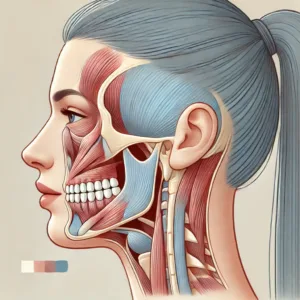
Trigeminovascular System
The trigeminovascular system plays a crucial role in migraine pathophysiology. It comprises:
- Peripheral components: Trigeminal nerve fibers innervating cranial blood vessels and meninges.
- Central components: Trigeminal nucleus caudalis in the brainstem and higher-order pain processing centers.
During a migraine attack, activation of the trigeminovascular system leads to the release of vasoactive neuropeptides, such as calcitonin gene-related peptide (CGRP), which contribute to neurogenic inflammation and pain sensitization.
Brainstem and Diencephalic Nuclei
Several brainstem and diencephalic structures are involved in modulating pain signals and controlling the trigeminovascular system. These include:
- Periaqueductal gray (PAG): Involved in descending pain modulation.
- Locus coeruleus: A major source of noradrenergic projections in the brain.
- Raphe nuclei: Important for serotonergic neurotransmission.
- Hypothalamus: Regulates various physiological functions and has been implicated in the prodromal phase of migraine.
Dysfunction in these regions may contribute to the altered pain processing and associated symptoms observed in migraine.
Cortical Spreading Depression
Cortical spreading depression (CSD) is a wave of neuronal and glial depolarization that spreads across the cortex. It is believed to underlie the aura phase of migraine and may also play a role in triggering the headache phase. CSD is characterized by:
- A slowly propagating wave of depolarization (2-6 mm/min) across the cortex.
- Transient disruption of ionic gradients and neurotransmitter release.
- Changes in cerebral blood flow and metabolism.
CSD has been shown to activate trigeminal nociceptors and may contribute to the activation of the trigeminovascular system.
Neurotransmitters and Neuropeptides in Migraine
Several neurotransmitters and neuropeptides are implicated in migraine pathophysiology:
Serotonin (5-HT)
Serotonin plays a critical role in pain signaling and modulation. Alterations in serotonergic neurotransmission have been observed in migraine patients, including:
- Changes in platelet serotonin levels during and between attacks.
- Altered expression of serotonin receptors in various brain regions.
- The effectiveness of serotonin receptor agonists (triptans) in treating migraine attacks.
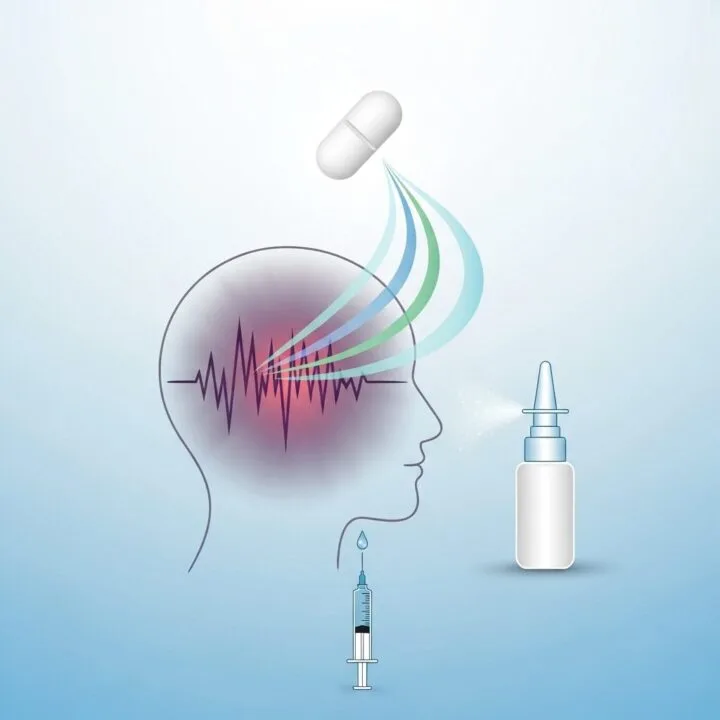
Calcitonin Gene-Related Peptide (CGRP)
CGRP is a key neuropeptide involved in migraine pathophysiology. Its release contributes to neurogenic inflammation and vasodilation. Evidence supporting the role of CGRP in migraine includes:
- Elevated CGRP levels in the external jugular vein during migraine attacks.
- Induction of migraine-like headaches by CGRP infusion in susceptible individuals.
- The effectiveness of CGRP receptor antagonists (gepants) and monoclonal antibodies targeting CGRP or its receptor in migraine treatment.
Glutamate
Glutamate, the primary excitatory neurotransmitter in the central nervous system, has been implicated in migraine pathophysiology. Alterations in glutamatergic neurotransmission may contribute to:
- Cortical hyperexcitability observed in migraine patients.
- The initiation and propagation of cortical spreading depression.
- Central sensitization of pain pathways.
Phases of Migraine: A Neurobiological Perspective
Migraine attacks typically progress through several distinct phases, each with its own underlying pathophysiology:
Prodrome Phase
The prodrome phase precedes the headache by up to 72 hours and involves:
- Activation of the hypothalamus, as evidenced by neuroimaging studies.
- Alterations in neurotransmitter levels, particularly dopamine and serotonin.
- Changes in homeostatic functions, leading to symptoms such as food cravings, mood changes, and fatigue.
Aura Phase
The aura phase, experienced by approximately 30% of migraine sufferers, is characterized by:
- Cortical spreading depression, which underlies the neurological symptoms of aura.
- Activation of trigeminal afferents, potentially linking the aura to the subsequent headache phase.
- Changes in blood-brain barrier permeability, which may facilitate the entry of pain-inducing substances into the central nervous system.
Headache Phase
The headache phase involves:
- Activation of the trigeminovascular system, leading to the release of vasoactive neuropeptides.
- Release of inflammatory mediators, contributing to neurogenic inflammation.
- Sensitization of peripheral and central pain pathways, resulting in hyperalgesia and allodynia.
Postdrome Phase
The postdrome phase shares similarities with the prodrome phase and may involve:
- Persistent alterations in brain activity, as observed in functional neuroimaging studies.
- Lingering symptoms such as fatigue, cognitive difficulties, and mood changes.
- Gradual resolution of the neurochemical and physiological changes that occurred during the attack.
Neuroimaging Insights into Migraine Pathophysiology
Advanced neuroimaging techniques have provided valuable insights into the structural and functional changes associated with migraine. Key findings include:
- Alterations in gray and white matter structure in regions involved in pain processing and sensory integration.
- Functional connectivity changes in pain-related brain networks, both during and between migraine attacks.
- Evidence of hypothalamic activation in the early stages of a migraine attack, supporting its role in attack initiation.
These neuroimaging findings have helped refine our understanding of migraine as a complex brain disorder involving multiple neural networks and systems.
Conclusion: Migraine as a Disorder of Sensory Processing
The current view of migraine pathophysiology emphasizes its nature as a disorder of sensory processing, with the brain exhibiting altered responses to various internal and external stimuli. This perspective integrates the genetic, neuroanatomical, and neurochemical aspects of migraine, providing a comprehensive framework for understanding its complex symptomatology.Key points in this integrated view include:
- Genetic factors predispose individuals to altered brain function and sensory processing.
- Dysfunction in brainstem and diencephalic modulatory systems leads to abnormal regulation of sensory inputs.
- Activation of the trigeminovascular system and release of inflammatory mediators contribute to pain and associated symptoms.
- Cortical spreading depression underlies the aura phase and may trigger subsequent phases of the attack.
- Alterations in multiple neurotransmitter systems, particularly serotonin, CGRP, and glutamate, play crucial roles throughout the migraine cycle.
Understanding the complex pathophysiology of migraine has led to the development of novel therapeutic approaches, including CGRP-targeted treatments and neuromodulation techniques. As research continues to unravel the intricacies of migraine biology, there is hope for even more effective and personalized treatment strategies in the future.:
Goadsby, P. J., Holland, P. R., Martins-Oliveira, M., Hoffmann, J., Schankin, C., & Akerman, S. (2017). Pathophysiology of migraine: a disorder of sensory processing. Physiological reviews, 97(2), 553-622.:
Ferrari, M. D., Klever, R. R., Terwindt, G. M., Ayata, C., & van den Maagdenberg, A. M. (2015). Migraine pathophysiology: lessons from mouse models and human genetics. The Lancet Neurology, 14(1), 65-80.:
Noseda, R., & Burstein, R. (2013). Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain, 154, S44-S53.:
Charles, A. C., & Baca, S. M. (2013). Cortical spreading depression and migraine. Nature Reviews Neurology, 9(11), 637-644.:
Hamel, E. (2007). Serotonin and migraine: biology and clinical implications. Cephalalgia, 27(11), 1293-1300.:
Edvinsson, L., Haanes, K. A., Warfvinge, K., & Krause, D. N. (2018). CGRP as the target of new migraine therapies—successful translation from bench to clinic. Nature Reviews Neurology, 14(6), 338-350.:
Pietrobon, D., & Moskowitz, M. A. (2014). Chaos and commotion in the wake of cortical spreading depression and spreading depolarizations. Nature Reviews Neuroscience, 15(6), 379-393.:
Maniyar, F. H., Sprenger, T., Monteith, T., Schankin, C., & Goadsby, P. J. (2014). Brain activations in the premonitory phase of nitroglycerin-triggered migraine attacks. Brain, 137(1), 232-241.:
Giffin, N. J., Lipton, R. B., Silberstein, S. D., Olesen, J., & Goadsby, P. J. (2016). The migraine postdrome: An electronic diary study. Neurology, 87(3), 309-313.: Schulte, L. H., & May, A. (2016). The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain, 139(7), 1987-1993.









Post Comment