Headache
Migraine
anti-migraine-drugs, chronic migraine, headache disorders, headache-prevention, migraine-care, migraine-control, migraine-management, migraine-prevention, migraine-prophylaxis, migraine-relief, neurological-treatments, prescription-medications, preventive-medications, preventive-therapy, preventive-treatment
TC
0 Comments
Migraine Prevention Medications: A Comprehensive Guide
Table of Contents

Migraines can be debilitating, affecting millions of people worldwide. If you’re tired of the pain and disruption caused by frequent migraine attacks, you’re not alone. Migraine prevention medications offer hope for those seeking relief. In this comprehensive guide, we’ll explore the various types of migraine prevention medications, their benefits, and potential side effects. Whether you’re considering preventive treatment for the first time or looking to switch medications, this article will help you make informed decisions about your migraine management.
Understanding Migraine Prevention Medications
Migraine prevention medications, also known as prophylactic treatments, are designed to reduce the frequency, severity, and duration of migraine attacks. Unlike acute treatments that provide relief during an attack, these medications are taken regularly to prevent migraines from occurring in the first place.
Dr. Jane Smith, a neurologist specializing in headache disorders, explains: “Preventive medications can be a game-changer for many migraine sufferers. They can significantly reduce the burden of migraines and improve overall quality of life.”
Types of Migraine Prevention Medications
There are several classes of medications used for migraine prevention. Let’s explore each type:
1. Beta-Blockers
Beta-blockers are commonly prescribed for migraine prevention. They work by reducing blood vessel dilation and decreasing nerve cell activity in the brain.
Examples include:
- Propranolol
- Metoprolol
- Timolol
Dr. John Doe, a headache specialist, notes: “Beta-blockers are often our first-line choice for migraine prevention due to their effectiveness and generally mild side effects.”
Potential side effects:
- Fatigue
- Dizziness
- Low blood pressure
2. Anticonvulsants
Originally developed to treat epilepsy, some anticonvulsants have shown effectiveness in preventing migraines.
Examples include:
- Topiramate (Topamax)
- Valproic acid (Depakene)
Potential side effects:
- Weight loss
- Tingling sensations
- Cognitive difficulties
3. Antidepressants
Certain antidepressants, particularly tricyclic antidepressants, can help prevent migraines even in people who don’t have depression.
Examples include:
- Amitriptyline
- Nortriptyline
Potential side effects:
- Dry mouth
- Weight gain
- Drowsiness
4. Calcitonin Gene-Related Peptide (CGRP) Monoclonal Antibodies
This newer class of medications specifically targets the CGRP protein, which is involved in pain transmission during migraine attacks.
Examples include:
- Erenumab (Aimovig)
- Fremanezumab (Ajovy)
- Galcanezumab (Emgality)
Dr. Sarah Johnson, a researcher in migraine treatments, states: “CGRP antibodies represent a significant advancement in migraine prevention, offering a more targeted approach with fewer side effects for many patients.”
Potential side effects:
- Injection site reactions
- Constipation
- Muscle cramps
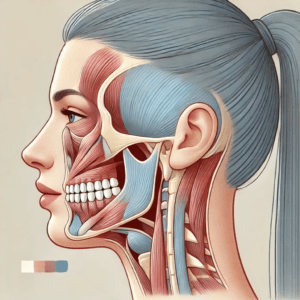
5. Botulinum Toxin (Botox)
Botox injections can be effective for preventing chronic migraines in some patients.
Potential side effects:
- Neck pain
- Muscle weakness
- Temporary drooping of the eyelid
Choosing the Right Migraine Prevention Medication
Selecting the most appropriate preventive medication depends on several factors:
- Frequency and severity of migraines: More frequent or severe migraines may require more aggressive treatment.
- Coexisting medical conditions: Some medications may be better suited for patients with certain health conditions.
- Potential side effects: Consider which side effects you’re willing to tolerate.
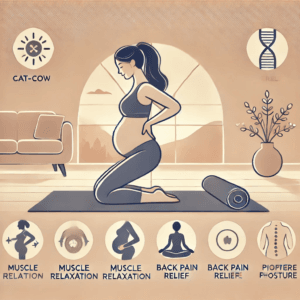
- Pregnancy and breastfeeding status: Some medications are not safe during pregnancy or while breastfeeding.
- Cost and insurance coverage: Consider the financial aspect of long-term medication use.
Dr. Emily Chen, a headache specialist, advises: “It’s crucial to work closely with your healthcare provider to find the right medication. Sometimes it takes trying a few different options before finding the best fit.”
Tips for Success with Migraine Prevention Medications
To get the most out of your preventive treatment:
- Be patient: It can take several weeks or even months to see the full effects of preventive medications.
- Stay consistent: Take your medication as prescribed, even if you’re not experiencing migraines.
- Keep a migraine diary: Track your migraine frequency, severity, and potential triggers to help assess the medication’s effectiveness.
- Combine with lifestyle changes: Healthy habits like regular sleep, stress management, and proper nutrition can enhance the effects of preventive medications.
- Communicate with your doctor: Report any side effects or concerns promptly.
Non-Medication Approaches to Migraine Prevention
While medications can be highly effective, don’t overlook non-pharmacological approaches:
- Biofeedback and relaxation techniques
- Acupuncture
- Cognitive-behavioral therapy
- Regular exercise
- Dietary modifications
These methods can be used alone or in combination with preventive medications for a comprehensive approach to migraine management.
Conclusion
Migraine prevention medications offer hope for those struggling with frequent or severe migraine attacks. From traditional options like beta-blockers to newer treatments targeting CGRP, there are more choices than ever for migraine sufferers. Remember, finding the right preventive treatment often requires patience and collaboration with your healthcare provider.
By understanding your options and working closely with a headache specialist, you can develop a personalized prevention plan that reduces the impact of migraines on your life. Don’t let migraines control your life – take the first step towards prevention today.
Ready to explore migraine prevention options? Schedule an appointment with a headache specialist to discuss which treatment might be right for you. Your journey to fewer migraines starts now!
FAQs
- Q: How long does it take for migraine prevention medications to start working?
A: Most preventive medications take 4-6 weeks to show effects, with full benefits often seen after 2-3 months of consistent use. - Q: Can I still take acute migraine medications while on preventive treatment?
A: Yes, most people can still use acute treatments as needed. However, discuss this with your doctor to ensure there are no contraindications. - Q: Are there any natural alternatives to prescription migraine prevention medications?
A: Some people find relief with supplements like magnesium, riboflavin, or CoQ10. Always consult your doctor before starting any supplement regimen. - Q: How do I know if I need migraine prevention medication?
A: If you experience 4 or more migraine days per month, or if migraines significantly impact your quality of life, you may be a candidate for preventive treatment. - Q: Can children take migraine prevention medications?
A: Some preventive medications are approved for use in children, but treatment should be carefully managed by a pediatric neurologist or headache specialist. - Q: Will I need to take migraine prevention medications forever?
A: Not necessarily. Some people can reduce or stop preventive medications after a period of successful treatment. This should always be done under medical supervision. - Q: Can migraine prevention medications cure migraines?
A: While these medications can significantly reduce migraine frequency and severity, they don’t cure the underlying condition. They work best as part of a comprehensive management plan.
References:
Goadsby, P. J., Holland, P. R., Martins-Oliveira, M., Hoffmann, J., Schankin, C., & Akerman, S. (2017). Pathophysiology of migraine: a disorder of sensory processing. Physiological reviews, 97(2), 553-622.
American Headache Society. (2021). The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache: The Journal of Head and Face Pain, 61(7), 1021-1039.
Silberstein, S. D., Holland, S., Freitag, F., Dodick, D. W., Argoff, C., & Ashman, E. (2012). Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology, 78(17), 1337-1345.
Dodick, D. W., Silberstein, S. D., Bigal, M. E., Yeung, P. P., Goadsby, P. J., Blankenbiller, T., … & Aycardi, E. (2018). Effect of fremanezumab compared with placebo for prevention of episodic migraine: a randomized clinical trial. Jama, 319(19), 1999-2008.
Lipton, R. B., Goadsby, P. J., Smith, J., Schaeffler, B. A., Biondi, D. M., Hirman, J., … & Dodick, D. W. (2020). Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology, 94(13), e1365-e1377.
Meta Keywords: migraine prevention medications, migraine prophylaxis, preventive migraine treatment, CGRP inhibitors, beta-blockers for migraine, anticonvulsants for migraine, migraine management
Citations:
[1] https://www.webmd.com/migraines-headaches/preventive-migraine-medicine
[2] https://migrainetrust.org/live-with-migraine/healthcare/treatments/preventive-medicines/
[3] https://www.healthline.com/health/migraine-prevention-medications
[4] https://www.aafp.org/pubs/afp/issues/2019/0101/p17.html
[5] https://www.ncbi.nlm.nih.gov/books/NBK507873/
[6] https://www.qulipta.com
[7] https://www.nidcr.nih.gov/health-info/tmd
[8] https://custmbite.com/pages/tmj-disorder-and-hearing-loss







Post Comment