What Are Migraine Aura Triggers and How Do You Avoid Them
Table of Contents

What Are Migraine Aura Triggers and How Do You Avoid Them?
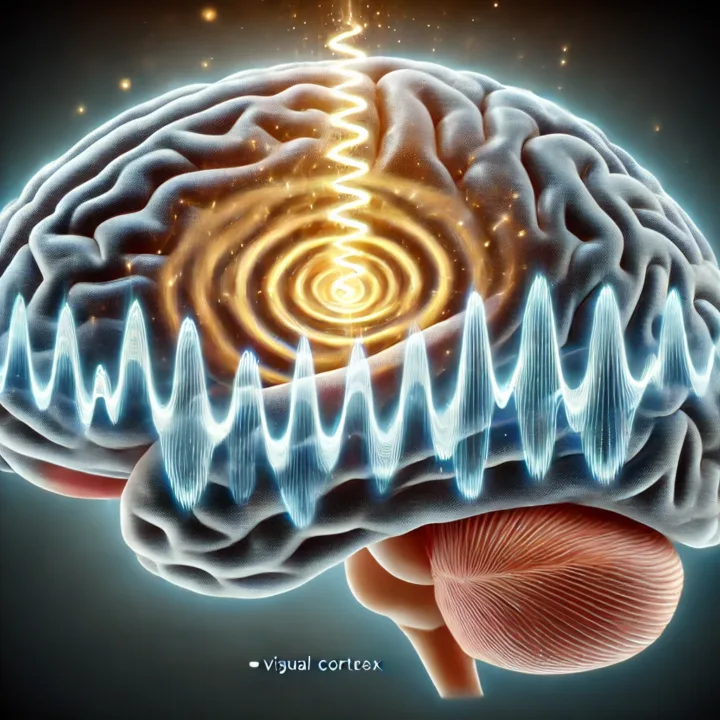
Migraines are tough enough on their own, but add an aura—visual distortions, numbness, or speech problems—and daily life can grind to a halt. Some people see flashy zigzag lines; others endure pins-and-needles sensations or a wave of disorientation. These symptoms often warn that a painful headache is on the way, though aura can also occur by itself. Understanding which factors spark these episodes is crucial. When you know your triggers, you can make lifestyle changes to reduce how often and how severe they strike.
Common Migraine Aura Triggers
Stress and Emotional Turmoil
Stressful workdays, sudden life changes, or anxiety can set the stage for migraine aura. Your body releases stress hormones that disturb normal nerve activity, making migraines more likely. Chronic stress amplifies this effect, so it’s vital to manage tension before it builds.
Tips
- Schedule daily “wind-down” periods or short breaks.
- Practice deep breathing or guided imagery.
- Consider journaling to identify patterns between stress levels and migraines.
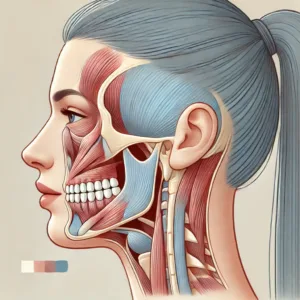
Sensory Overload
Bright lights, glaring screens, loud noises, or intense odors can overwhelm the nervous system. For many migraine-prone individuals, an environment rich in such stimuli can trigger aura swiftly.
Tips
- Wear sunglasses outdoors or in fluorescent lighting.
- Dim electronic screens and reduce screen time.
- Limit exposure to strong scents like perfumes or heavy chemicals.
Hormonal Shifts
Changes in estrogen—common during menstrual cycles, pregnancy, or menopause—can increase aura frequency in some women. The body’s fluctuating hormone levels create an internal climate ripe for migraines.
Tips
- Track your cycle to spot patterns in aura occurrence.
- Discuss hormonal treatments or adjustments with a healthcare provider.
- Maintain balanced nutrition and regular exercise, both of which stabilize hormones.
Dietary Influences
Some foods, beverages, or additives act as migraine aura triggers. Common suspects include aged cheeses, chocolate, red wine, and processed meats. Caffeine can help certain migraines but can also provoke symptoms if consumed excessively or withdrawn abruptly.
Tips
- Keep a food diary to match specific meals or snacks with subsequent aura episodes.
- Moderate rather than eliminate possible triggers to avoid abrupt changes.
- Stay hydrated, since dehydration can intensify headaches and aura symptoms.
Sleep Disturbances
Erratic sleep schedules, insomnia, or oversleeping throw off the body’s internal clock. This disruption can ignite migraine aura, as the brain struggles to regulate sensory processing and pain perception when fatigued.
Tips
- Keep a consistent bedtime and wake-up time, even on weekends.
- Limit blue light exposure before bed by reducing screen use.
- Consider gentle stretches or relaxing music to prepare the mind for rest.
Strategies to Prevent Migraine Aura
Identify Personal Patterns
Each person reacts differently to triggers. Using a migraine journal or tracking app helps pinpoint factors—diet, stress, environment, hormones—that correlate with your aura. Over time, these entries reveal your unique vulnerabilities, guiding you toward the most impactful lifestyle adjustments.
Practice Mind-Body Techniques
Regular yoga, meditation, or tai chi can calm an overstimulated nervous system and curb stress-induced attacks. Even short sessions of focused breathing can ground you when you sense an aura coming on.
Stabilize Blood Sugar
Skipping meals or overloading on refined carbs leads to blood sugar spikes and crashes, which can provoke migraines. Aim for balanced meals with protein, fiber, and healthy fats, and avoid extreme hunger or overeating.
Use Medications Consistently
If you have prescription medication for migraines or aura, follow the schedule your doctor recommends. Inconsistent use can trigger rebound headaches or unpredictable aura patterns. Some doctors might also prescribe preventive drugs that lower migraine intensity or frequency.
Conclusion
Migraines with aura are not just painful; they can be disorienting and disruptive. Recognizing migraine aura triggers lets you adopt preventive measures—whether that means lowering stress, tweaking your diet, or improving sleep routines. Relief isn’t always immediate, but consistent effort offers real hope. As you track patterns and fine-tune your approach, episodes may become shorter, less frequent, or easier to manage. Work with your healthcare provider for added support, and remember that small changes can add up to significant improvements in your daily life.
FAQ
1. Can I have aura without a headache?
Yes. Known as a silent migraine, aura symptoms may appear without the typical throbbing pain.
2. Are migraines with aura hereditary?
Genes can increase your risk. If migraines run in your family, you may be more prone to them, though lifestyle factors also play a role.
3. Do over-the-counter meds help with aura?
They can lessen migraine pain but may not always stop aura. Consult a doctor for personalized advice, especially if aura impacts daily activities.
4. Are natural remedies like magnesium effective for aura?
Magnesium and other supplements benefit some people, though effectiveness varies. Always speak to a healthcare professional before adding new supplements.
5. When should I seek medical help for changing aura symptoms?
If your aura suddenly worsens, lasts longer than usual, or presents entirely new signs (like severe weakness), see a healthcare provider to rule out other conditions.








Post Comment