Is Nerve Pain a Sign of Fibromyalgia? Here’s What to Know
Table of Contents

Is Nerve Pain a Sign of Fibromyalgia? Here’s What to Know
Are you experiencing widespread pain, tingling sensations, and extreme sensitivity to touch? You might be wondering if these symptoms point to fibromyalgia or nerve pain. Let’s dive into the complex world of fibromyalgia and its connection to nerve pain.
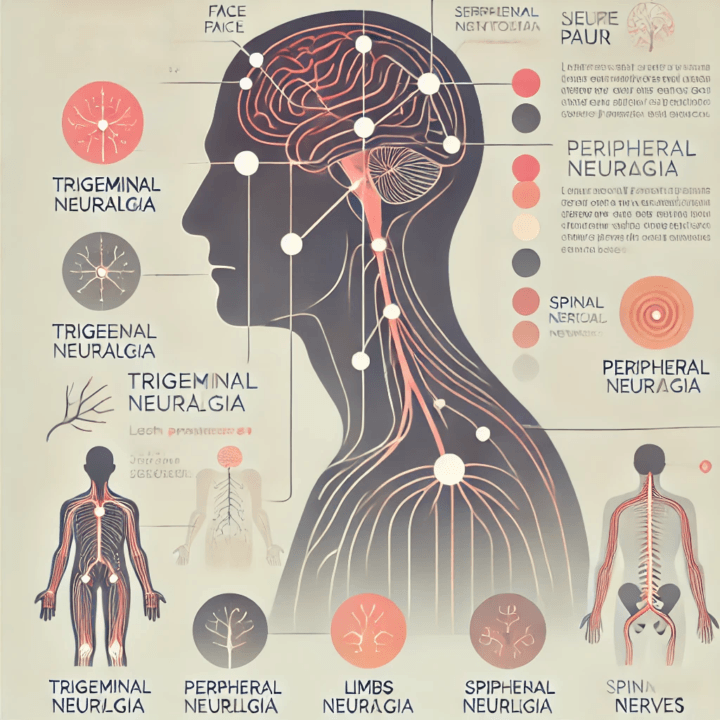
Understanding Fibromyalgia and Nerve Pain
Fibromyalgia is a chronic condition characterized by widespread pain, fatigue, and cognitive issues. But is nerve pain a sign of fibromyalgia? The short answer is: it can be.
Many people with fibromyalgia experience symptoms that resemble nerve pain, including burning sensations, tingling, and numbness. This has led researchers to investigate the link between fibromyalgia and nerve-related disorders.
The Fibromyalgia-Nerve Pain Connection
Recent studies have shed light on the relationship between fibromyalgia and nerve pain. It turns out that the connection is more complex than we once thought.
Central Sensitization: The Brain’s Pain Amplifier
Fibromyalgia is believed to involve central sensitization, a condition where the central nervous system becomes hypersensitive to pain signals[1]. Imagine your brain’s volume control for pain being stuck on high. That’s what central sensitization feels like.
This hypersensitivity can make even mild stimuli feel painful. A light touch might feel like a hard pinch. A cool breeze could feel like ice on your skin. It’s as if your body’s alarm system is constantly going off, even when there’s no real danger.
Small Fiber Neuropathy: A Possible Culprit
Here’s where things get interesting. Some researchers now suspect that many people with fibromyalgia might actually have a condition called small fiber neuropathy (SFN)[2].
SFN is a type of nerve damage that affects the small nerve fibers in your skin. These fibers are responsible for sensing pain and temperature. When they’re damaged, you might experience symptoms that are remarkably similar to fibromyalgia:
- Burning pain
- Tingling sensations
- Numbness
- Extreme sensitivity to touch
In fact, studies have found that 30-50% of people with fibromyalgia show signs of SFN[3]. That’s a pretty significant overlap!
Diagnosing Fibromyalgia and Nerve Pain
Now, you might be thinking, “How can I tell if I have fibromyalgia, nerve pain, or both?” Great question! Let’s break down the diagnostic process.
Fibromyalgia Diagnosis: More Than Just Tender Points
In the past, doctors used to diagnose fibromyalgia by checking for specific tender points on the body. But we’ve come a long way since then.
Today, fibromyalgia diagnosis is based on a combination of factors:
- Widespread pain lasting at least 3 months
- Presence of other symptoms like fatigue and cognitive issues
- Absence of other conditions that could explain the symptoms
Doctors might use questionnaires to assess your symptoms and their impact on your daily life. They’ll also perform a physical exam and may order blood tests to rule out other conditions.
Nerve Pain Diagnosis: Looking for the Root Cause
Diagnosing nerve pain, or neuropathy, involves a different approach. Doctors will typically:
- Take a detailed medical history
- Perform a neurological exam
- Order tests like nerve conduction studies or skin biopsies
For suspected SFN, a skin biopsy can reveal if you have reduced nerve fiber density in your skin[4]. This test can be particularly helpful in distinguishing between fibromyalgia and SFN.
Treatment Options: Tackling Fibromyalgia and Nerve Pain
Whether you’re dealing with fibromyalgia, nerve pain, or a combination of both, there are treatment options available. Let’s explore some of the most effective approaches.
Medications: Finding the Right Balance
Several types of medications can help manage fibromyalgia and nerve pain symptoms:
- Antidepressants: Drugs like duloxetine and milnacipran can help reduce pain and improve mood.
- Anti-seizure medications: Pregabalin and gabapentin are often used to treat nerve pain.
- Pain relievers: Over-the-counter pain medications can help manage mild to moderate pain.
Remember, what works for one person might not work for another. It’s all about finding the right combination for you.
Lifestyle Changes: Small Steps, Big Impact
Medications aren’t the only tool in your arsenal. Lifestyle changes can make a big difference:
- Exercise: Regular, gentle exercise can help reduce pain and improve mood. Start small and gradually increase your activity level.
- Sleep hygiene: Good sleep is crucial for managing pain. Establish a regular sleep schedule and create a relaxing bedtime routine.
- Stress management: Techniques like meditation, deep breathing, or yoga can help reduce stress and pain.
Alternative Therapies: Exploring Your Options
Many people find relief through alternative therapies:
- Acupuncture: Some studies suggest acupuncture can help reduce fibromyalgia pain.
- Massage therapy: Gentle massage may help relieve muscle tension and pain.
- Cognitive Behavioral Therapy (CBT): This type of therapy can help you develop coping strategies for dealing with chronic pain.
Living with Fibromyalgia and Nerve Pain: It’s Possible!
Living with chronic pain isn’t easy, but it’s important to remember that you’re not alone. Millions of people around the world are navigating similar challenges.
Here are some tips for managing day-to-day life:
- Pace yourself: Break tasks into smaller, manageable chunks. It’s okay to take breaks!
- Communicate: Let your loved ones know how you’re feeling. They can’t help if they don’t understand.
- Find your tribe: Connect with others who have similar experiences. Support groups can be a great source of information and encouragement.
- Stay positive: Focus on what you can do, not what you can’t. Celebrate small victories!
Remember, managing fibromyalgia and nerve pain is a journey, not a destination. Be patient with yourself and don’t hesitate to reach out for help when you need it.
Conclusion
Is nerve pain a sign of fibromyalgia? It certainly can be. The relationship between fibromyalgia and nerve pain is complex, with conditions like small fiber neuropathy blurring the lines even further.
If you’re experiencing symptoms of widespread pain, fatigue, and sensitivity, it’s important to consult with a healthcare professional. They can help determine whether you’re dealing with fibromyalgia, nerve pain, or both, and work with you to develop an effective treatment plan.
Remember, while living with chronic pain can be challenging, it’s not impossible. With the right combination of treatments, lifestyle changes, and support, many people with fibromyalgia and nerve pain lead fulfilling, active lives. You’ve got this!
FAQs
- Can fibromyalgia cause permanent nerve damage?
While fibromyalgia itself doesn’t cause permanent nerve damage, some people with fibromyalgia may have an underlying condition like small fiber neuropathy that can lead to nerve damage if left untreated. - How can I tell if my pain is from fibromyalgia or nerve damage?
It can be difficult to distinguish between fibromyalgia pain and nerve pain on your own. A healthcare professional can perform specific tests to determine the source of your pain. - Are there any natural remedies for fibromyalgia nerve pain?
Some people find relief from natural remedies like gentle exercise, meditation, and certain dietary changes. However, it’s important to discuss any new treatments with your doctor. - Can stress make fibromyalgia nerve pain worse?
Yes, stress can exacerbate fibromyalgia symptoms, including nerve pain. Stress management techniques can be an important part of managing fibromyalgia. - Is fibromyalgia considered a disability?
Fibromyalgia can be considered a disability if it significantly impacts your ability to work or perform daily activities. However, qualifying for disability benefits can be challenging and often requires extensive documentation.













Post Comment