Digestive Health
Natural Remedies
acid reflux diet, acid reflux treatment, antacids benefits, digestive health, esophageal health, GERD management, healthy eating for acid reflux, heartburn prevention tips, heartburn symptoms, heartburn-friendly meals, lifestyle changes for heartburn relief, natural remedies for heartburn, proton pump inhibitors, stress management for digestion
TC
0 Comments
Heartburn Symptoms and Treatment: Comprehensive Insights for Lasting Relief
Table of Contents
Heartburn Symptoms and Treatment: Comprehensive Insights for Lasting Relief
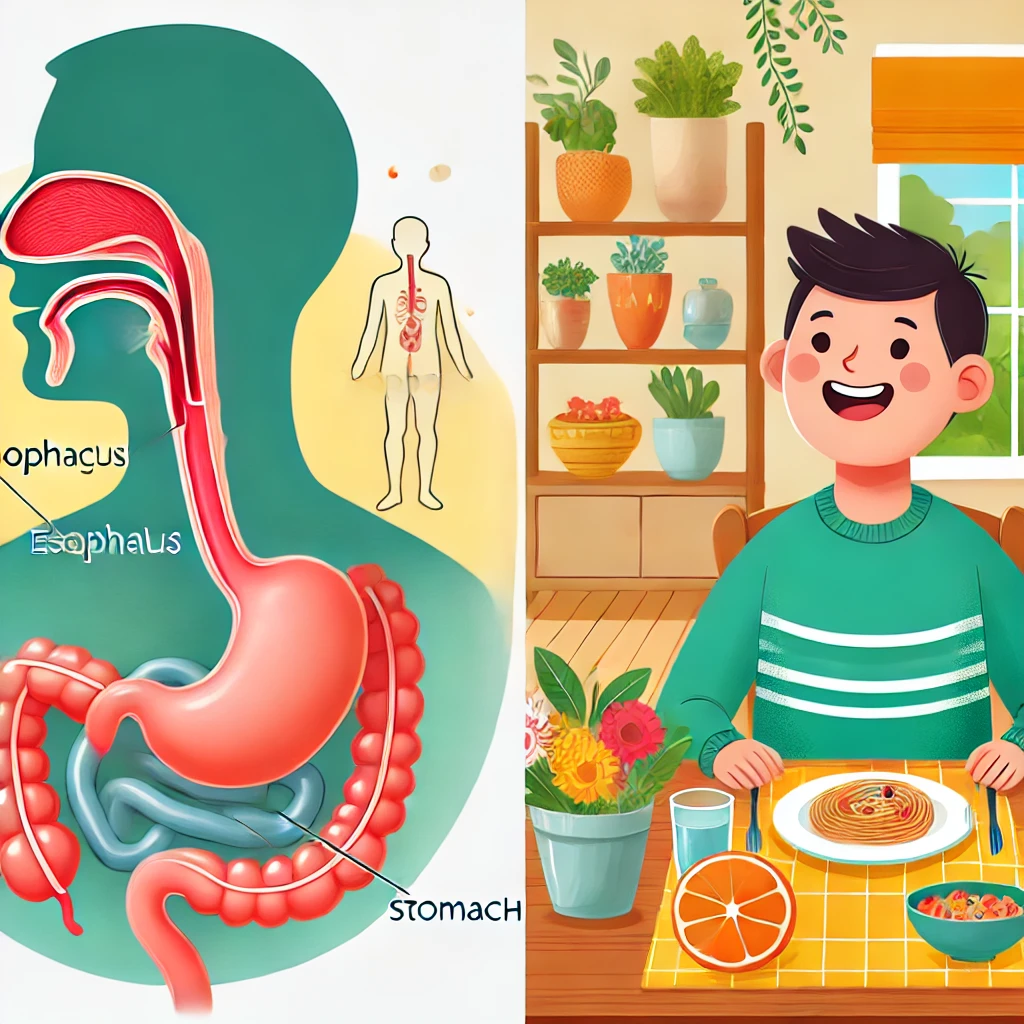
Heartburn—that familiar and uncomfortable burning sensation in the chest—is a condition many experience, but few fully understand. Caused by stomach acid flowing back into the esophagus, heartburn, or acid reflux, disrupts the delicate balance of the digestive system. Beyond occasional discomfort, chronic heartburn can significantly impact quality of life, interfering with sleep, productivity, and emotional well-being. This guide explores the nuanced symptoms of heartburn, delves into its underlying causes, and outlines evidence-based treatments and prevention strategies tailored to a deeper academic understanding.
Understanding Heartburn Symptoms
Heartburn symptoms encompass a spectrum of discomforts, ranging in intensity and frequency. Key indicators include:
- Burning Sensation in the Chest: Characterized by a sharp, localized pain often felt behind the sternum, this symptom is typically exacerbated by eating or reclining shortly afterward.
- Sour or Bitter Taste: Resulting from acid reaching the back of the throat, this sensation often accompanies regurgitation.
- Odynophagia (Painful Swallowing): A sensation of obstruction or pain when swallowing, often signaling esophageal irritation.
- Laryngopharyngeal Reflux (LPR): Hoarseness, persistent cough, or the sensation of a lump in the throat may result from reflux affecting the larynx.
- Nocturnal Symptoms: Symptoms that worsen when lying down, interrupting sleep and indicating increased esophageal exposure to acid during recumbency.
Chronic symptoms often point to gastroesophageal reflux disease (GERD), a condition requiring both lifestyle adjustments and medical intervention.
Causes and Contributing Factors of Heartburn
A multidimensional analysis reveals diverse triggers and risk factors for heartburn, including:
- Gastrointestinal Anatomy and Function: Dysfunction of the lower esophageal sphincter (LES) is a primary contributor, allowing acid to escape the stomach.
- Dietary Triggers: Foods high in fat, spices, or acidity can lower LES pressure or increase gastric acidity.
- Behavioral Patterns: Late-night meals, excessive portion sizes, or insufficient mastication can exacerbate reflux episodes.
- Physiological Conditions: Obesity, pregnancy, and hiatal hernias alter intra-abdominal pressure dynamics, predisposing individuals to reflux.
- Pharmacological Interactions: Drugs such as NSAIDs, calcium channel blockers, or sedatives may exacerbate LES dysfunction or mucosal irritation.
Evidence-Based Treatment Approaches
The management of heartburn integrates a combination of lifestyle modifications, dietary refinements, pharmacological treatments, and complementary interventions. Below is a layered approach:
1. Dietary and Behavioral Strategies
- Trigger Avoidance: Eliminate or minimize the intake of reflux-inducing substances, such as citrus, tomatoes, caffeine, and alcohol.
- Meal Structuring: Prioritize smaller, frequent meals over large portions to alleviate gastric pressure.
- Pre-Sleep Practices: Conclude eating at least three hours before reclining and consider ergonomic sleeping solutions, such as inclined sleeping positions.
2. Therapeutic Lifestyle Modifications
- Weight Management: Obesity amplifies intra-abdominal pressure, while modest weight loss has been shown to mitigate reflux frequency and severity.
- Tobacco Cessation: Smoking weakens the LES and exacerbates mucosal damage, necessitating cessation as a cornerstone of treatment.
- Stress Reduction Techniques: Cognitive-behavioral therapy (CBT), progressive muscle relaxation, and mindfulness meditation are increasingly recognized for their role in alleviating gastrointestinal distress.
3. Pharmacological Interventions
- Antacids: Neutralize gastric acidity, offering rapid but transient relief.
- H2 Receptor Blockers: Agents like ranitidine or famotidine suppress acid secretion, suitable for moderate, episodic symptoms.
- Proton Pump Inhibitors (PPIs): These potent inhibitors, including omeprazole and esomeprazole, are gold-standard treatments for chronic reflux, although long-term usage should be monitored for risks like nutrient malabsorption.
4. Innovative and Integrative Remedies
- Aloe Vera Extracts: Demonstrated anti-inflammatory properties benefit esophageal mucosal healing.
- Functional Foods and Probiotics: Emerging research links specific strains of Lactobacillus to improved gut motility and acid regulation.
- Acupuncture: Preliminary evidence suggests benefits in reducing reflux symptoms via neuromodulatory effects.
5. Criteria for Advanced Evaluation
Persistent symptoms unresponsive to standard care warrant further diagnostic workup, including endoscopy or pH monitoring, to rule out Barrett’s esophagus, strictures, or other complications.
Preventative Strategies for Long-Term Control
Preventing recurrent heartburn involves proactive, sustainable strategies:
- Nutritional Tracking: Maintaining a food and symptom diary facilitates individualized identification of triggers.
- Hydration Practices: Sufficient water intake supports enzymatic processes and prevents exacerbation of acidity.
- Physical Activity: Moderate exercise, particularly postprandial walks, can enhance gastrointestinal motility.
- Thermal Therapy: Warm compresses or relaxation aids may reduce stress-related exacerbations.
Conclusion
Understanding and managing heartburn is both an art and a science, requiring a holistic approach that integrates lifestyle, pharmacological, and complementary treatments. For students and professionals alike, delving into the interplay of physiology, behavior, and nutrition reveals not only a roadmap for relief but a framework for broader gastroenterological health. Persistent cases underscore the importance of medical collaboration to ensure optimal outcomes.











Post Comment