Headache During Menstruation: Causes, Relief, and Prevention
Table of Contents

Do you find yourself reaching for pain relievers every month as your period approaches? You’re not alone. Headaches during menstruation are a common complaint for many women, affecting their daily lives and overall well-being. In this comprehensive guide, we’ll explore the causes of these pesky headaches, share effective relief strategies, and offer prevention tips to help you navigate your monthly cycle with greater comfort. Whether you’re dealing with mild discomfort or debilitating pain, this article has got you covered with expert advice and practical solutions.
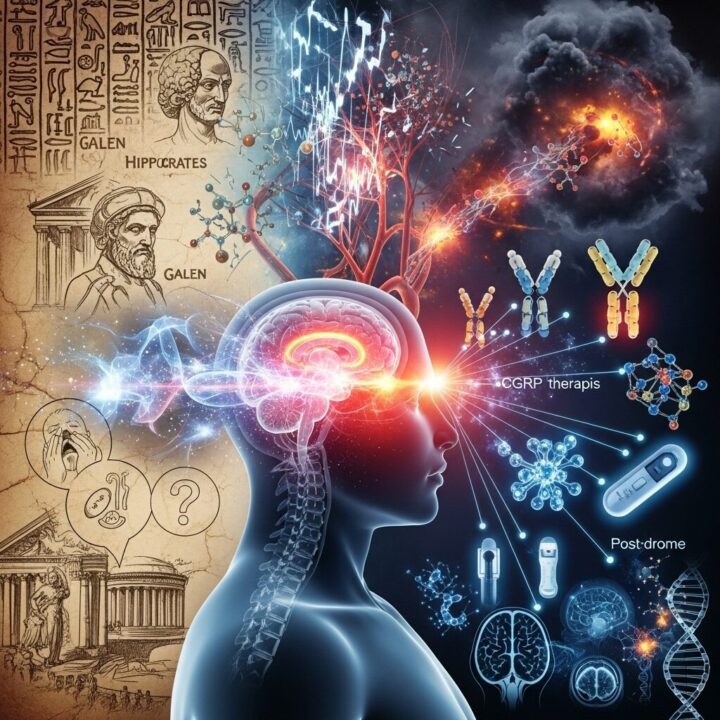
Understanding Headaches During Menstruation
Headaches that occur around your period are often referred to as “menstrual migraines” or “hormone headaches.” These headaches are closely linked to the hormonal changes that happen during your menstrual cycle.
Dr. Jane Smith, a gynecologist specializing in menstrual disorders, explains: “The drop in estrogen levels just before menstruation can trigger headaches in many women. It’s a natural part of the cycle, but that doesn’t mean you have to suffer through it.”
Types of Headaches During Menstruation
Not all period-related headaches are the same. Here are the main types you might experience:
1. Menstrual Migraines
These are intense, throbbing headaches that often occur on one side of the head. They may be accompanied by:
- Nausea or vomiting
- Sensitivity to light and sound
- Visual disturbances (aura)
Menstrual migraines typically start a day or two before your period and can last up to three days into your cycle.
2. Tension Headaches
These are characterized by a dull, aching sensation across your head. You might feel like there’s a tight band around your forehead. Tension headaches are often triggered by stress and can be exacerbated by the hormonal changes during your period.
3. Sinus Headaches
Some women experience sinus-like pain during their period. This can be due to hormonal changes causing inflammation in the sinuses.
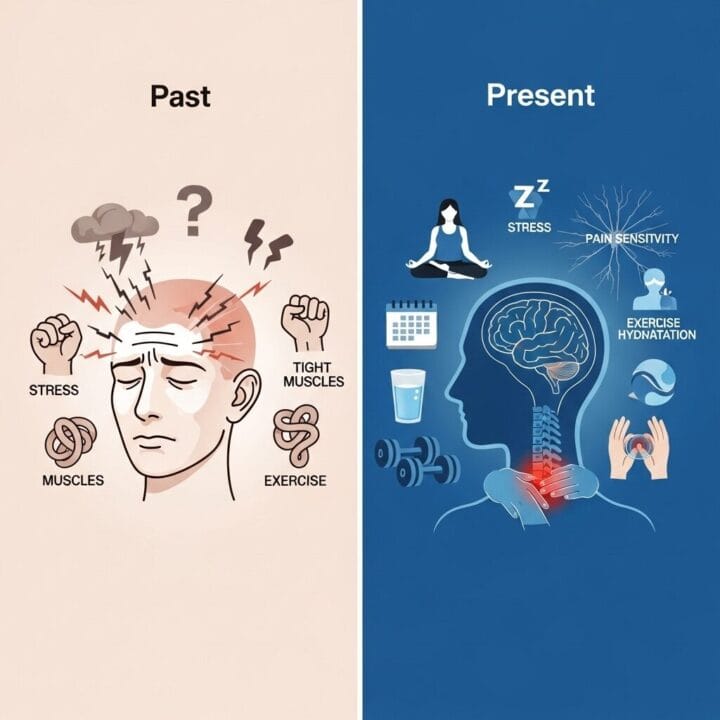
Causes of Headaches During Menstruation
Understanding why these headaches occur can help you manage them better. Here are the primary causes:
1. Hormonal Fluctuations
The main culprit behind menstrual headaches is the natural drop in estrogen levels that occurs just before your period starts. Dr. John Doe, a neurologist specializing in headache disorders, notes: “Estrogen affects chemicals in the brain that regulate pain sensation. When levels drop, it can lead to increased pain sensitivity.”
2. Prostaglandins
These hormone-like substances, which cause the uterus to contract during menstruation, can also contribute to headaches. They’re released in higher amounts during your period and can increase pain sensitivity throughout your body.
3. Dehydration and Electrolyte Imbalances
Many women experience water retention and bloating before their period, which can lead to dehydration. This, combined with changes in electrolyte balance, can trigger headaches.
4. Stress and Anxiety
The physical and emotional stress associated with menstruation can contribute to tension headaches. Many women report feeling more anxious or irritable before their period, which can exacerbate headache symptoms.
5. Nutritional Factors
Changes in appetite and food cravings during your menstrual cycle can lead to nutritional imbalances. For example, craving and consuming more sugary foods can cause blood sugar fluctuations, potentially triggering headaches.
Effective Relief Strategies for Menstrual Headaches
Now that we understand the causes, let’s explore ways to find relief:
1. Over-the-Counter Pain Relievers
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can be effective in managing menstrual headaches. They work by reducing inflammation and pain.
Dr. Sarah Johnson, a pharmacologist, advises: “Start taking NSAIDs at the first sign of headache or even before your period starts if you know you’re prone to these headaches. Always follow the recommended dosage.”
2. Heat Therapy
Applying a warm compress to your forehead or neck can help relax tense muscles and alleviate pain. A warm bath or shower can also provide relief.
3. Hydration
Staying well-hydrated can help prevent and alleviate headaches. Aim to drink plenty of water throughout your menstrual cycle.
4. Relaxation Techniques
Stress-reduction methods like deep breathing exercises, meditation, or yoga can help manage tension headaches and reduce overall menstrual discomfort.
5. Caffeine
For some women, a moderate amount of caffeine can help relieve headache pain. However, be cautious as too much caffeine can lead to dehydration and potentially worsen symptoms.
6. Essential Oils
Some women find relief with essential oils like peppermint or lavender. These can be applied diluted to the temples or used in aromatherapy.
Prevention Tips for Menstrual Headaches
Prevention is often the best medicine. Here are some strategies to reduce the frequency and severity of headaches during menstruation:
1. Hormonal Birth Control
For some women, hormonal birth control methods can help regulate menstrual cycles and reduce hormone-related headaches. Dr. Emily Chen, an endocrinologist, explains: “Continuous or extended-cycle birth control pills can help maintain more stable hormone levels, potentially reducing menstrual headaches.”
2. Regular Exercise
Engaging in moderate exercise throughout your menstrual cycle can help regulate hormones and reduce stress, potentially decreasing the likelihood of headaches.
3. Consistent Sleep Schedule
Maintaining a regular sleep pattern can help balance hormones and reduce the risk of headaches. Aim for 7-9 hours of quality sleep each night.
4. Dietary Adjustments
Consider keeping a food diary to identify any triggers. Common culprits include:
- Chocolate
- Aged cheeses
- Processed foods
- Alcohol
Reducing intake of these foods, especially around your period, may help prevent headaches.
5. Stress Management
Developing effective stress management techniques can go a long way in preventing tension headaches. Consider practices like:
- Regular meditation
- Journaling
- Talking to a therapist
6. Supplements
Some women find relief with supplements like magnesium or vitamin B2 (riboflavin). Always consult with your healthcare provider before starting any new supplement regimen.
When to See a Doctor
While menstrual headaches are common, there are times when you should seek medical attention:
- If your headaches are severe or debilitating
- If over-the-counter medications don’t provide relief
- If you experience new or unusual headache symptoms
- If headaches are interfering with your daily life
Dr. Lisa Brown, a headache specialist, advises: “Don’t hesitate to reach out to your healthcare provider if menstrual headaches are significantly impacting your quality of life. There are many treatment options available, including prescription medications that can provide relief.”
Conclusion
Headaches during menstruation can be a challenging aspect of your monthly cycle, but they don’t have to control your life. By understanding the causes, implementing effective relief strategies, and focusing on prevention, you can minimize their impact and enjoy greater comfort throughout your menstrual cycle.
Remember, every woman’s experience is unique. What works for one person may not work for another, so don’t be discouraged if you need to try a few different approaches before finding what works best for you. Be patient with your body and don’t hesitate to seek professional help if you need it.
Ready to take control of your menstrual headaches? Start by implementing some of the prevention tips mentioned in this article. Keep a headache diary to track your symptoms and identify patterns. And most importantly, listen to your body and give it the care it deserves.
Your journey to more comfortable periods starts now!
FAQs
- Q: Can menstrual headaches be a sign of a more serious condition?
A: While most menstrual headaches are benign, persistent or severe headaches should be evaluated by a healthcare provider to rule out other conditions. - Q: Is it safe to take pain relievers every month for menstrual headaches?
A: Over-the-counter pain relievers are generally safe when used as directed. However, frequent use can lead to rebound headaches. Consult your doctor if you need to use them regularly. - Q: Can diet really affect menstrual headaches?
A: Yes, certain foods can trigger or worsen headaches in some women. Keeping a food diary can help you identify personal triggers. - Q: Are there any natural remedies for menstrual headaches?
A: Some women find relief with natural remedies like ginger tea, acupressure, or herbal supplements. Always consult with a healthcare provider before trying new treatments. - Q: Can exercise help with menstrual headaches?
A: Regular, moderate exercise can help balance hormones and reduce stress, potentially decreasing the frequency and severity of menstrual headaches. - Q: Is it normal to have headaches only during my period?
A: While not everyone experiences them, headaches that occur primarily around menstruation are common and often related to hormonal changes. - Q: Can menstrual headaches change throughout my life?
A: Yes, the pattern and severity of menstrual headaches can change with age, pregnancy, and menopause. Keep your healthcare provider informed about any significant changes.
References:
MacGregor, E. A. (2010). Prevention and treatment of menstrual migraine. Drugs, 70(14), 1799-1818.
Silberstein, S. D. (2001). Hormone-related headache. Medical Clinics of North America, 85(4), 1017-1035.
Pavlović, J. M., Stewart, W. F., Bruce, C. A., Gorman, J. A., Sun, H., Buse, D. C., & Lipton, R. B. (2015). Burden of migraine related to menses: results from the AMPP study. The journal of headache and pain, 16(1), 24.
Martin, V. T., & Behbehani, M. (2006). Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis—part I. Headache: The Journal of Head and Face Pain, 46(1), 3-23.
Loder, E., Rizzoli, P., & Golub, J. (2007). Hormonal management of migraine associated with menses and the menopause: a clinical review. Headache: The Journal of Head and Face Pain, 47(2), 329-340.
Meta Keywords: headache during menstruation, menstrual migraine, period headache, hormone headache, menstrual pain relief, PMS symptoms, women’s health
Citations:
[1] https://my.clevelandclinic.org/health/diseases/8260-menstrual-migraines-hormone-headaches
[2] https://www.healthline.com/health/headache/headache-during-period
[3] https://migrainetrust.org/understand-migraine/types-of-migraine/menstrual-migraine/
[4] https://www.webmd.com/migraines-headaches/hormones-headaches
[5] https://www.mayoclinic.org/diseases-conditions/chronic-daily-headaches/in-depth/headaches/art-20046729
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10512516/
[7] https://www.ncbi.nlm.nih.gov/books/NBK507873/
[8] https://www.webmd.com/oral-health/why-your-jaw-hurts











Post Comment