Headache Diagnosis Guide: How Doctors Pinpoint Your Pain Source
Table of Contents
As a neurologist who has spent years studying and treating headache disorders, I’ve come to appreciate the complexity and nuance involved in diagnosing these often debilitating conditions. Headaches, while ubiquitous, are far from simple. The process of pinpointing the exact source of a patient’s head pain is akin to solving a intricate puzzle, with each piece of information bringing us closer to a clear picture.
The Art and Science of Headache Diagnosis
Diagnosing headaches is both an art and a science. It requires a delicate balance of clinical acumen, patient history, and, when necessary, advanced diagnostic tools. The journey to diagnosis often begins with a simple question: “Tell me about your headache.” This open-ended inquiry can reveal a wealth of information that guides our diagnostic process.
The Crucial Role of Patient History
In my experience, a thorough patient history is the cornerstone of headache diagnosis. We delve into various aspects of the headache experience:
- Frequency and duration of headaches
- Pain characteristics (throbbing, pressing, stabbing)
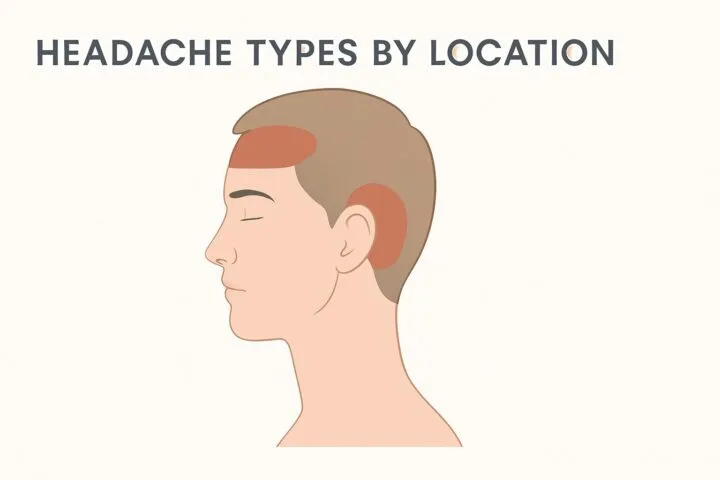
- Location of pain
- Associated symptoms (nausea, light sensitivity, visual disturbances)
- Triggers and alleviating factors
- Impact on daily life
This detailed history allows us to begin categorizing the headache into broad types such as tension-type, migraine, or cluster headaches.
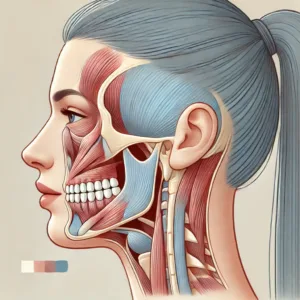
Physical Examination: Beyond the Head
While headaches primarily manifest as head pain, a comprehensive physical examination is crucial. We assess neurological function, check for signs of increased intracranial pressure, and evaluate the head and neck muscles. Sometimes, clues to a headache’s origin lie in unexpected places, like tight cervical muscles or subtle neurological deficits.
Diagnostic Criteria: The ICHD-3
In the realm of headache medicine, the International Classification of Headache Disorders, 3rd edition (ICHD-3) is our bible. This comprehensive guide provides specific diagnostic criteria for over 200 headache types. For instance, a diagnosis of migraine without aura requires at least five attacks fulfilling specific criteria related to duration, pain characteristics, and associated symptoms.
When to Consider Advanced Imaging
While most primary headaches (like tension-type and migraines) don’t require imaging, there are red flags that prompt us to consider CT scans or MRIs:
- Sudden onset of severe headache
- New onset of headache after age 50
- Changes in headache pattern or intensity
- Neurological deficits or seizures
- Headache associated with systemic symptoms
These imaging studies help rule out secondary causes of headache, such as tumors, aneurysms, or other structural abnormalities.
The Role of Headache Diaries
I often recommend that patients keep a headache diary for at least a month. This tool provides invaluable insights into patterns, triggers, and the effectiveness of treatments. In the age of smartphones, numerous apps make this process more convenient than ever.
Specialized Tests for Complex Cases
In some cases, we may employ specialized tests:
- Lumbar puncture to measure cerebrospinal fluid pressure
- Sleep studies for suspected sleep apnea-related headaches
- Allergy tests for suspected sinus-related headaches
These tests are typically reserved for complex cases or when initial treatments prove ineffective.
The Diagnostic Journey: A Collaborative Process
It’s important to understand that headache diagnosis is often an iterative process. The initial diagnosis may evolve as we gather more information or observe response to treatments. I always emphasize to my patients that this is a collaborative journey. Their active participation in tracking symptoms, identifying triggers, and providing feedback on treatments is crucial to reaching an accurate diagnosis and effective management plan.
When to Seek Immediate Medical Attention
While most headaches are not life-threatening, there are situations that warrant immediate medical attention:
- The “worst headache of your life”
- Headache accompanied by fever, stiff neck, or rash
- Headache following a head injury
- Sudden onset of headache with neurological symptoms
These scenarios could indicate serious conditions like meningitis, subarachnoid hemorrhage, or stroke, requiring urgent evaluation.
Conclusion: The Path to Personalized Headache Management
Accurate diagnosis is the foundation of effective headache management. It allows us to tailor treatments to the specific type of headache and the individual patient’s needs. As our understanding of headache disorders continues to evolve, so too do our diagnostic and treatment approaches.
If you’re struggling with recurrent or severe headaches, don’t hesitate to seek medical evaluation. With the right diagnosis, we can develop a management plan that not only alleviates pain but improves overall quality of life. Remember, you don’t have to navigate this journey alone – healthcare professionals are here to guide you towards a life with fewer and less severe headaches.








Post Comment