Can Physical Therapy Help with Temporomandibular Joint Disorder? 🤔
Table of Contents

Can Physical Therapy Help with Temporomandibular Joint Disorder? 🤔
Introduction
Have you ever experienced that annoying, sometimes painful clicking in your jaw when you open your mouth wide or take a big bite of your favorite food? You’re not alone. Many people worry that such persistent jaw discomfort could be temporomandibular joint disorder (often shortened to TMJ or TMD). Questions swirl: “Is it serious?” “Can it progress?” “Will I need surgery?” These concerns are valid. After all, the temporomandibular joint (TMJ) is crucial for everyday activities like speaking, chewing, and even yawning.
That’s where physical therapy steps in as a less invasive, often highly effective approach. In a world where jaw pain can significantly impact your quality of life—from disrupted meal times to tense facial muscles—knowing your options empowers you to take control. Can physical therapy help with temporomandibular joint disorder? Absolutely. In this blog post, we’ll dissect what TMJ disorder is, explore how physical therapy can offer relief, and provide actionable tips to help you manage symptoms and possibly prevent flare-ups. By the end, you’ll understand how strategic exercises, posture adjustments, and other supportive therapies can make a real difference. Let’s dive in and uncover how to get that jaw back on track.
What Exactly Is Temporomandibular Joint Disorder?
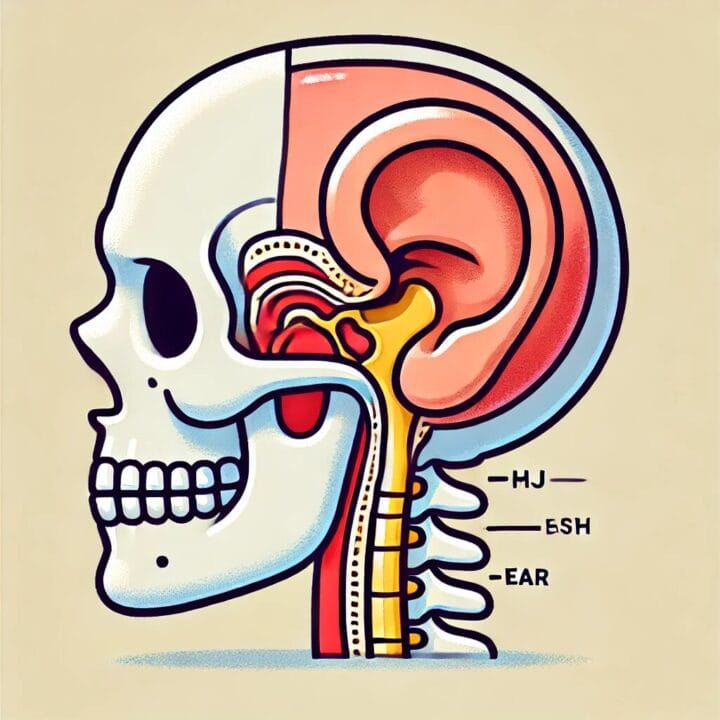
The temporomandibular joint is the hinge connecting your jaw to your skull. This joint, supported by muscles, ligaments, and an articular disc, allows you to move your jaw up, down, and side-to-side. Temporomandibular joint disorder (TMD) occurs when there’s a malfunction or strain in these structures. Common culprits include teeth grinding (bruxism), jaw misalignment, trauma, arthritis, or chronic stress. Symptoms often manifest as facial pain, restricted jaw movement, and even headaches or earaches. If these issues are left unresolved, they can escalate, impacting your ability to chew, speak, or enjoy normal day-to-day activities. The good news? Early interventions—particularly physical therapy—can offer significant relief and help restore normal function without resorting to more invasive procedures.
How Does Physical Therapy Address TMJ Problems?
Physical therapy tackles TMD by focusing on muscle balance, joint movement, and pain relief. A trained physical therapist starts with a thorough assessment of your jaw alignment, neck posture, and jaw mobility. Here’s how they typically help:
- Manual Techniques: Gentle mobilization can help realign the jaw, ease muscle tension, and reduce inflammation. These hands-on methods may also target neck and upper-back muscles, which often contribute to jaw stress.
- Targeted Exercises: Physical therapists guide you through specific jaw exercises—like opening and closing movements or controlled lateral shifts. These exercises strengthen supportive muscles, promote flexibility, and alleviate pain over time.
- Postural Training: Believe it or not, slouching or prolonged head-forward posture strains the jaw. Correcting your posture helps evenly distribute muscle tension, relieving undue stress on the TMJ.
- Pain Management Modalities: Therapists may incorporate ultrasound, heat, cold therapy, or low-level laser treatments to relax stiff muscles and reduce inflammation. This combined approach speeds recovery and curbs symptom severity.
By identifying specific biomechanical issues and customizing a rehab plan, physical therapy addresses root causes rather than masking symptoms. It’s a proactive strategy that promotes long-term relief and improved jaw function.
What To Expect During Physical Therapy Sessions
Your first appointment usually involves a detailed evaluation. You’ll discuss your history of jaw pain, any popping or clicking sounds, and daily habits (like teeth grinding or gum chewing). The physical therapist then checks your jaw’s range of motion, muscle tightness, and possible trigger points.
A Typical Session May Include:
- Gentle Manual Therapy: Techniques to stretch or massage tight muscles around the jaw and neck.
- Exercises and Stretches: Focused moves that strengthen or relax specific muscle groups.
- Posture Corrections: Guidance on how to keep your head, shoulders, and spine aligned throughout the day.
- Home Exercise Program: You’ll receive instructions for daily exercises and tips to manage flare-ups (e.g., applying warm compresses at home).
Many people notice improvements in a few sessions, although longer-standing TMD may require more sustained therapy. Consistency is key. By sticking with prescribed exercises and being mindful of posture, you can accelerate your recovery and reduce the likelihood of future jaw issues.
Lifestyle Adjustments to Complement Physical Therapy
Physical therapy works best when combined with smart lifestyle choices:
- Stress Management: Techniques like deep breathing or short meditation sessions help mitigate jaw clenching caused by tension or anxiety.
- Diet Modifications: Opt for softer foods during flare-ups to avoid overworking the jaw.
- Sleep Position: Sleeping on your back (rather than your stomach) can reduce pressure on the jaw. Consider supportive pillows to keep the neck and spine aligned.
- Mouthguards: If nighttime bruxism is an issue, a professionally fitted mouthguard can lessen wear on the TMJ.
- Hydration: Staying well-hydrated helps maintain muscle elasticity, potentially easing jaw stiffness.
These steps, paired with physical therapy, create a holistic approach to healing. They not only relieve current symptoms but also prevent recurring discomfort, making day-to-day activities easier and more enjoyable.
Conclusion
So, can physical therapy help with temporomandibular joint disorder? The answer is a resounding yes. From manual joint mobilizations to targeted exercises, a physical therapist can craft a personalized program that reduces pain, improves jaw mobility, and addresses underlying causes of TMJ dysfunction. In many cases, these therapies also integrate seamlessly with lifestyle adjustments—like stress management and posture correction—to offer comprehensive relief. While TMD can be bothersome, it doesn’t have to be a lifelong struggle. With proactive care and consistent follow-through, you can alleviate jaw tension, decrease discomfort, and restore normal function. In essence, physical therapy doesn’t just manage TMJ symptoms; it empowers you to take control of your health and enjoy life without constant jaw pain.
FAQ ❓
- Is it ever too late to start physical therapy for TMJ issues?
Not at all. Whether your TMJ problems are recent or long-standing, therapy can help restore function and ease pain. - How long does it take to see results?
Many patients notice reduced jaw pain and improved movement in a few weeks, but severity and consistency in following exercises affect the timeline. - Do I need a referral to see a physical therapist for TMJ?
This depends on your location and insurance plan. Contact your insurer or local healthcare provider to confirm. - Will insurance cover my physical therapy sessions?
Coverage varies. Some plans cover TMJ-related therapy under their standard physical therapy benefits. Check with your provider. - Are there any self-massage techniques I can do at home?
Yes! Gentle circular motions along the jaw muscles and light stretching can help. Always consult your therapist for guidance.











Post Comment