Best Medicines for TMJ Flare-Ups: Expert-Recommended Relief
Table of Contents

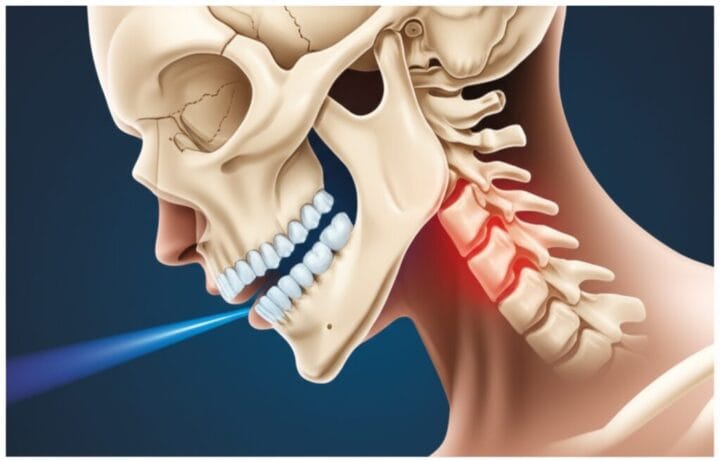
If you’ve ever experienced the sharp, shooting pain of a TMJ flare-up, you know how desperately you want relief. Temporomandibular joint (TMJ) disorders can cause intense discomfort, making everyday activities like eating and talking a real challenge. In this comprehensive guide, we’ll explore the best medicines for TMJ flare-ups, from over-the-counter options to prescription drugs. We’ll also share expert tips on managing your symptoms and preventing future flare-ups. So, let’s dive in and find the relief you’ve been searching for!
Over-the-Counter Options for Quick Relief
When a TMJ flare-up strikes, your first line of defense is often the medicine cabinet at home or your local pharmacy. Here are some effective over-the-counter (OTC) options:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are the go-to choice for many TMJ sufferers. They work by reducing inflammation and pain in the jaw area. Popular options include:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve)
- Aspirin
Pro tip: For best results, take NSAIDs at the first sign of a flare-up. This can help nip the pain in the bud before it gets worse.
2. Acetaminophen
While it doesn’t reduce inflammation like NSAIDs, acetaminophen (Tylenol) can still be effective for pain relief. It’s a good alternative if you can’t take NSAIDs due to stomach issues or other health concerns.
3. Topical Pain Relievers
Don’t overlook the power of topical treatments! Creams or gels containing ingredients like menthol or capsaicin can provide localized relief when applied to the jaw area. Look for products specifically designed for muscle and joint pain.
Prescription Medications for Stubborn TMJ Pain
If OTC options aren’t cutting it, it might be time to talk to your doctor about prescription medications. Here are some that have shown promise in treating TMJ flare-ups:
1. Muscle Relaxants
These medications can help ease tension in the jaw muscles, providing relief from pain and stiffness. Common options include:
- Cyclobenzaprine (Flexeril)
- Metaxalone (Skelaxin)
- Tizanidine (Zanaflex)
Remember: Muscle relaxants can cause drowsiness, so it’s best to take them at night or when you don’t need to drive or operate machinery.
2. Prescription-Strength NSAIDs
For more severe pain, your doctor might prescribe stronger NSAIDs like:
- Celecoxib (Celebrex)
- Meloxicam (Mobic)
- Diclofenac (Voltaren)
These medications can be more effective than their OTC counterparts but may also come with a higher risk of side effects.
3. Tricyclic Antidepressants
Don’t let the name fool you – these medications aren’t just for depression. In low doses, tricyclic antidepressants like amitriptyline can help with chronic pain conditions, including TMJ disorders.
4. Corticosteroids
In some cases, your doctor might recommend a short course of oral corticosteroids like prednisone to quickly reduce inflammation and pain. These are typically reserved for severe flare-ups and aren’t suitable for long-term use.
Alternative and Complementary Treatments
While medications can provide quick relief, it’s worth exploring other treatment options to manage your TMJ pain:
1. Botox Injections
Botulinum toxin (Botox) injections can help relax the jaw muscles, potentially reducing pain and improving function. While not a first-line treatment, it’s an option worth discussing with your healthcare provider for chronic TMJ issues.
2. Acupuncture
Some people find relief from TMJ pain through acupuncture. While more research is needed, it’s a low-risk option that might be worth trying if other treatments haven’t worked.
3. Herbal Supplements
Certain herbs and supplements, like turmeric or omega-3 fatty acids, have anti-inflammatory properties that might help with TMJ pain. Always check with your doctor before starting any new supplements, especially if you’re taking other medications.
Lifestyle Changes to Prevent TMJ Flare-Ups
While medications can provide relief during a flare-up, preventing them in the first place is even better. Here are some tips to keep your jaw happy:
- Practice stress-reduction techniques like meditation or yoga
- Avoid chewy or hard foods during flare-ups
- Use proper posture, especially when working at a computer
- Wear a night guard if you grind your teeth in your sleep
- Apply heat or cold packs to your jaw for 10-15 minutes at a time
When to See a Doctor
While many TMJ flare-ups can be managed at home, there are times when professional help is necessary. Seek medical attention if:
- Your pain is severe or lasts more than a few days
- You have difficulty opening or closing your mouth
- You experience persistent clicking or popping sounds in your jaw
- Over-the-counter medications aren’t providing relief
Conclusion
Dealing with TMJ flare-ups can be frustrating, but with the right approach, you can find relief and get back to enjoying life. From over-the-counter pain relievers to prescription medications and lifestyle changes, there are many options to explore. Remember, what works best can vary from person to person, so don’t be afraid to try different approaches under your doctor’s guidance.
By combining effective medications with preventive measures, you can reduce the frequency and severity of your TMJ flare-ups. And always listen to your body – if something doesn’t feel right or your pain persists, don’t hesitate to reach out to a healthcare professional.
Here’s to finding the relief you deserve and saying goodbye to jaw pain!
FAQs
- Q: Can I take ibuprofen and acetaminophen together for TMJ pain?
A: Yes, it’s generally safe to take both, as they work differently in the body. However, always follow dosage instructions and consult your doctor if you have any concerns. - Q: How long does a typical TMJ flare-up last?
A: The duration can vary, but most flare-ups last a few days to a couple of weeks. If your pain persists longer, consult a healthcare provider. - Q: Are there any natural remedies for TMJ pain?
A: Yes, some people find relief with natural remedies like applying a warm compress, practicing jaw exercises, or using essential oils like lavender or peppermint. - Q: Can stress cause TMJ flare-ups?
A: Absolutely! Stress is a common trigger for TMJ pain, often leading to teeth clenching or jaw tightening. Stress management techniques can help prevent flare-ups. - Q: Is it safe to take muscle relaxants long-term for TMJ pain?
A: Long-term use of muscle relaxants isn’t typically recommended due to potential side effects and the risk of dependency. Always follow your doctor’s advice on medication use. - Q: Can TMJ pain go away on its own?
A: In some cases, mild TMJ pain may resolve on its own with rest and self-care. However, persistent or severe pain should be evaluated by a healthcare professional. - Q: Are there any foods I should avoid during a TMJ flare-up?
A: Yes, it’s best to avoid hard, chewy, or crunchy foods during a flare-up. Stick to soft foods that don’t require much jaw movement, like smoothies, soups, and well-cooked vegetables.
Author Bio:
Dr. Emily Chen, DDS, is a board-certified orofacial pain specialist with over 15 years of experience treating TMJ disorders. She completed her residency at the UCLA Orofacial Pain Program and has published numerous articles on TMJ management in peer-reviewed journals. Dr. Chen is passionate about helping patients find relief from jaw pain and improving their quality of life.
References:
Gauer, R. L., & Semidey, M. J. (2015). Diagnosis and treatment of temporomandibular disorders. American family physician, 91(6), 378-386.
List, T., & Jensen, R. H. (2017). Temporomandibular disorders: Old ideas and new concepts. Cephalalgia, 37(7), 692-704.
Wieckiewicz, M., Boening, K., Wiland, P., Shiau, Y. Y., & Paradowska-Stolarz, A. (2015). Reported concepts for the treatment modalities and pain management of temporomandibular disorders. The Journal of Headache and Pain, 16(1), 106.
Häggman-Henrikson, B., Alstergren, P., Davidson, T., Högestätt, E. D., Östlund, P., Tranaeus, S., … & List, T. (2017). Pharmacological treatment of oro-facial pain – health technology assessment including a systematic review with network meta-analysis. Journal of oral rehabilitation, 44(10), 800-826.
Gil-Martínez, A., Paris-Alemany, A., López-de-Uralde-Villanueva, I., & La Touche, R. (2018). Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. Journal of pain research, 11, 571-587.
Citations:
[1] https://www.tmjtexas.com/medicine-for-tmj
[2] https://tmj.org/living-with-tmj/treatments/medications/
[3] https://www.raleightmjandsleep.com/what-is-the-best-treatment-for-tmj
[4] https://johnagarzadds.com/over-the-counter-muscle-relaxer-tmj/
[5] https://www.rickardschiropractic.com/jaw-pain-problem-among-pregnant-women/
[6] https://www.mayoclinic.org/diseases-conditions/tmj/diagnosis-treatment/drc-20350945
[7] https://www.webmd.com/oral-health/temporomandibular-disorders-tmd
[8] https://ostrowonline.usc.edu/medications-for-temporomandibular-disorders/












Post Comment