What Is Raynaud’s Syndrome and How Can You Manage It?
Table of Contents
What Is Raynaud’s Syndrome and How Can You Manage It?
Introduction
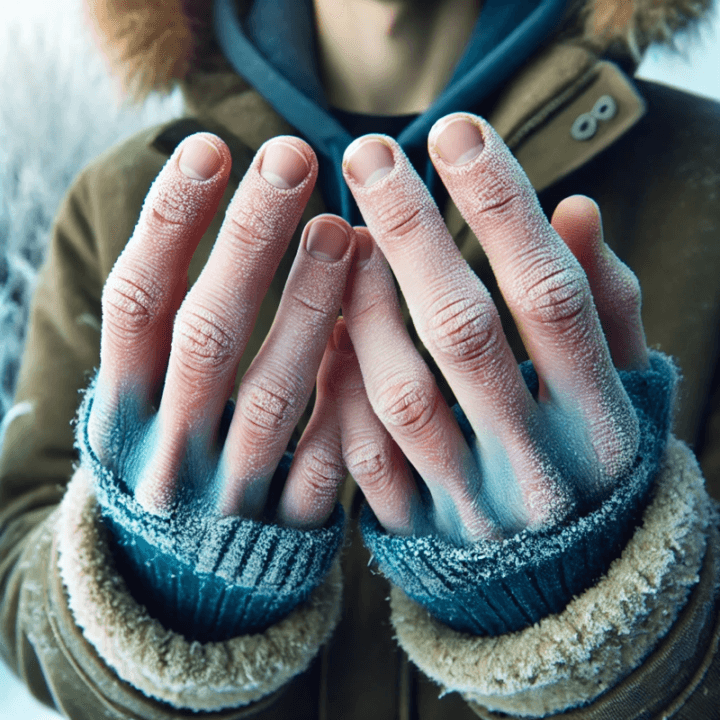
Have you ever stepped out into the cold, and within minutes, your fingers or toes turn white or blue and feel numb? You might have wondered: Is this normal, or could it be something serious? These episodes could be linked to a condition called Raynaud’s syndrome.
Raynaud’s syndrome, also known as Raynaud’s phenomenon, affects millions of people worldwide. While it’s often brushed off as a reaction to cold, it can signal deeper vascular issues. Understanding what causes Raynaud’s, its symptoms, and how to manage it can significantly improve your quality of life—especially if you live in colder regions or frequently experience stress.
Let’s dive into the science behind those cold, color-changing fingers and learn practical tips for controlling Raynaud’s attacks.
What Causes Raynaud’s Syndrome?
1. What Happens to the Blood Vessels During an Attack?
Raynaud’s syndrome occurs when small arteries in the extremities (fingers, toes, nose, and ears) suddenly narrow due to exaggerated vasoconstriction. This restricts blood flow, causing the affected areas to change color and lose sensation.
- Stage 1: Initially, the area turns white as blood flow is cut off.
- Stage 2: It often turns blue due to lack of oxygen.
- Stage 3: As blood flow returns, the skin may flush red and feel tingly or painful.
2. What Are the Primary Triggers?
Common triggers of Raynaud’s episodes include:
- Cold temperatures: Exposure to chilly weather or even holding a cold drink can trigger an attack.
- Stress or anxiety: Emotional stress can prompt a similar vasoconstrictive response.
- Vibration: Long-term exposure to vibrating tools (e.g., jackhammers) can exacerbate symptoms.
- Smoking: Nicotine constricts blood vessels, making symptoms worse.
What Are the Different Types of Raynaud’s?
1. What’s the Difference Between Primary and Secondary Raynaud’s?
- Primary Raynaud’s: This is the more common and generally milder form. It occurs independently without any underlying disease and usually develops between ages 15 and 30.
- Secondary Raynaud’s: This form is more severe and linked to other conditions such as lupus, scleroderma, or rheumatoid arthritis. It may lead to complications, including ulcers and tissue damage.
2. How Can You Tell the Two Apart?
Key differences:
- Primary Raynaud’s: Fewer complications, often triggered solely by cold or stress.
- Secondary Raynaud’s: Frequent, longer-lasting attacks and possible skin ulcers or infections due to reduced blood flow.
What Are the Symptoms of Raynaud’s Syndrome?
1. What Does a Typical Attack Feel Like?
A Raynaud’s attack can last anywhere from a few minutes to several hours. Common symptoms include:
- Cold, numb, or tingling fingers and toes.
- Skin discoloration (white, blue, and red stages).
- Burning or throbbing sensation as circulation returns.
- Difficulty performing tasks like buttoning a shirt due to temporary loss of dexterity.
2. Can It Affect Areas Beyond Fingers and Toes?
Yes, Raynaud’s can also affect:
- Nose and ears: Leading to cold, pale, or discolored skin.
- Lips: Brief discoloration during episodes.
How Can You Manage Raynaud’s Syndrome?
1. What Are Immediate Steps to Stop an Attack?
- Move to a warm environment as quickly as possible.
- Soak your hands or feet in warm water to restore circulation.
- Gently massage the affected area to encourage blood flow.
- Practice deep breathing exercises to reduce stress-induced attacks.
2. What Lifestyle Changes Can Help Prevent Attacks?
- Dress warmly: Wear gloves, thermal socks, and layered clothing when exposed to cold.
- Quit smoking: Nicotine worsens vasoconstriction.
- Exercise regularly: Improves circulation and overall vascular health.
- Manage stress: Practice meditation, yoga, or other relaxation techniques.
3. What Should You Include in Your Diet?
Certain foods can improve circulation and reduce inflammation:
- Omega-3 fatty acids: Found in fish like salmon and mackerel.
- Garlic: Known for its blood-thinning and circulation-boosting properties.
- Citrus fruits: Rich in vitamin C, which strengthens blood vessels.
When Should You See a Doctor?
1. What Are the Warning Signs of Severe Raynaud’s?
If you experience any of the following, seek medical attention:
- Frequent, prolonged attacks lasting more than an hour.
- Skin ulcers or sores that don’t heal.
- Severe pain or signs of infection.
2. What Tests Can Help Diagnose It?
- Nailfold capillaroscopy: A test that examines the capillaries near your fingernails to distinguish between primary and secondary Raynaud’s.
- Blood tests: To check for underlying autoimmune conditions.
3. What Medications Are Commonly Prescribed?
Depending on the severity, your doctor may recommend:
- Calcium channel blockers: To relax blood vessels and improve circulation.
- Vasodilators: To prevent or reduce the frequency of attacks.
- Topical nitrates: Applied to areas prone to attacks to promote blood flow.
What Are the Long-Term Solutions?
1. Can Biofeedback Help?
Biofeedback involves using electronic devices to monitor your body’s functions, like heart rate and temperature, helping you control and reduce stress-induced Raynaud’s episodes.
2. Is Surgery an Option?
In severe cases, a surgical procedure called sympathectomy can help by interrupting nerve signals that trigger vasoconstriction. However, this is usually a last resort.
Conclusion
Raynaud’s syndrome can be frustrating and painful, but it doesn’t have to control your life. By understanding the triggers, symptoms, and management techniques, you can significantly reduce the frequency and severity of attacks. Whether it’s dressing warmly, managing stress, or following a healthy diet, small changes can make a big difference.
If you experience frequent or severe symptoms, consult a healthcare professional to rule out underlying conditions. With the right care, Raynaud’s is manageable—and your hands and feet can stay warmer, longer.
FAQ
1. Can Raynaud’s syndrome go away on its own?
For some people, especially those with mild primary Raynaud’s, symptoms may diminish over time. However, secondary Raynaud’s usually requires long-term management.
2. Does Raynaud’s only happen in cold weather?
No, stress and other factors like handling cold objects or sudden temperature changes can also trigger episodes.
3. Can Raynaud’s cause permanent damage?
If left untreated, severe secondary Raynaud’s can lead to ulcers, infections, and tissue damage, though this is rare.
4. Are there natural remedies for Raynaud’s?
Natural remedies like ginger, ginkgo biloba, and omega-3 supplements may help improve circulation, but consult a doctor before trying any.
5. How is Raynaud’s syndrome diagnosed?
A combination of physical exams, nailfold capillaroscopy, and blood tests is commonly used to diagnose Raynaud’s and identify underlying conditions.












Post Comment