Is a TMJ Dental Splint Really the Answer? Understanding Effectiveness and What to Expect
Table of Contents
Is a TMJ Dental Splint Really the Answer? Understanding Effectiveness and What to Expect
Introduction
Are you waking up with a jaw that feels like it went ten rounds with Mike Tyson? Maybe you’re dealing with constant headaches, earaches that won’t quit, or a clicking jaw that sounds like a rusty hinge? If so, you’re probably wrestling with the frustrating reality of TMJ (temporomandibular joint) disorder, and you’re likely wondering about treatment options. One of the most common solutions thrown around is the TMJ dental splint – but does it actually work? Is it worth the investment? You’re probably thinking, “Will this thing finally give me some relief, or will it just be another gadget collecting dust on my nightstand?”
It’s a valid concern. After all, TMJ can be a real pain – not just in your jaw, but in your entire life. It can disrupt your sleep, make eating a chore, and just plain wear you down. So, let’s cut through the fluff and get real about what a TMJ dental splint can, and can’t, do for you. We’ll explore how they work, what the science says about their efficacy, different types, and what you should expect. No medical jargon or sales pitches, just honest, straightforward information to help you make the best decision for your health.
Understanding TMJ and Why a Splint is Considered
Your temporomandibular joint is like a hinge connecting your jawbone to your skull. It’s a complex joint, responsible for all the jaw movements you use every day – talking, chewing, yawning, the works. When this joint goes haywire, it causes a whole host of problems, ranging from mild discomfort to excruciating pain.
Causes of TMJ Disorder
Several factors can contribute to TMJ disorder, including:
- Bruxism (Teeth Grinding): Often occurring during sleep, grinding puts immense stress on the TMJ.
- Stress and Anxiety: Chronic stress can lead to jaw clenching and increased muscle tension.
- Bite Misalignment: When your teeth don’t align properly, it can strain the joint.
- Arthritis: Osteoarthritis or rheumatoid arthritis can affect the TMJ.
- Injury: Trauma to the jaw can result in TMJ disorder.
A TMJ dental splint is often recommended to alleviate these symptoms by stabilizing the bite and reducing clenching and grinding forces.
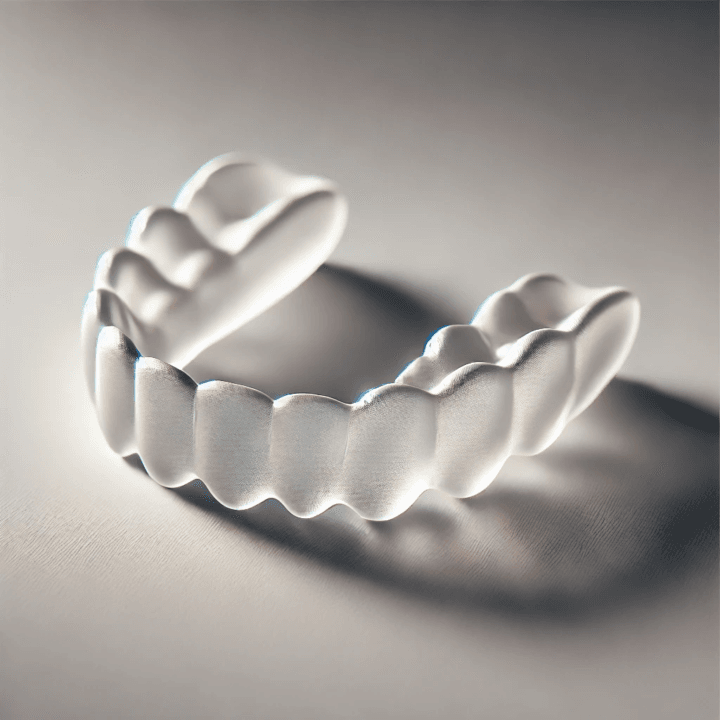
Different Types of TMJ Splints: What Are Your Options?
Not all splints are created equal. These devices are carefully crafted, and the type you get is crucial to its success. Let’s explore the various types available:
1. Stabilization Splints (Flat Plane Splints)
- Cover all teeth on the upper or lower jaw.
- Designed to provide an even contact surface to reduce clenching.
- Helps in muscle relaxation and pressure distribution.
2. Anterior Repositioning Splints
- Moves the jaw slightly forward to relieve pressure on the TMJ.
- Typically prescribed for short-term use.
3. Pivot Splints
- Less common, featuring small points of contact to minimize muscle activity.
- Limited research supporting their effectiveness.
4. NTI-tss Splints
- Covers only the front teeth to limit the intensity of jaw clenching.
- Studies have shown mixed results regarding effectiveness.
The Science Behind TMJ Splints: What Does the Research Say?
Scientific studies suggest that stabilization splints can help reduce TMJ-related pain and improve muscle function. Some key findings include:
- Pain Reduction: Splints can significantly reduce pain levels, particularly in the short term.
- Decreased Muscle Activity: They help reduce jaw muscle tension, preventing further damage.
- Improved Jaw Function: Many users report better jaw mobility and less discomfort.
However, long-term studies suggest that splints work best when combined with lifestyle modifications, such as stress management and physical therapy.
What to Expect When Getting a TMJ Splint
The process of obtaining and using a TMJ splint involves several steps:
- Initial Consultation: Your dentist will assess your symptoms and take impressions of your teeth.
- Fitting: Once the splint is custom-made, you’ll have a fitting appointment.
- Adjustment Period: Expect an adjustment period of 1-2 weeks to get used to wearing it.
- Follow-Up Visits: Regular check-ups are essential to ensure proper fit and effectiveness.
Maximizing Your TMJ Splint Effectiveness: Tips and Tricks
To get the most out of your TMJ splint, follow these guidelines:
- Wear it Consistently: Skipping nights can reduce its effectiveness.
- Maintain Good Oral Hygiene: Clean your splint daily to prevent bacteria buildup.
- Follow-Up Appointments: Regularly visit your dentist for adjustments.
- Consider Lifestyle Changes: Incorporate stress reduction techniques and a soft food diet when necessary.
Conclusion
A TMJ splint can be an effective solution for managing symptoms, but it’s not a one-size-fits-all approach. Combining it with other therapies and lifestyle changes can significantly enhance its effectiveness. Remember to work closely with your dentist to monitor progress and make adjustments as needed.
FAQ
Q1: How long will I need to wear a TMJ dental splint?
A: The duration varies, but most people wear them for several months to a year.
Q2: Can I buy an over-the-counter mouthguard instead?
A: No, custom-made splints are tailored to your specific needs, unlike generic mouthguards.
Q3: Will a TMJ splint permanently cure my condition?
A: It can alleviate symptoms, but addressing the root cause requires a holistic approach.











Post Comment